How Are Fertility Drugs for IVF Given?
April 20, 2025
How Long Is the IVF Process? Your Step-by-Step Guide to the Journey
April 20, 2025How Long Has IVF Been Around? A Deep Dive into Its History, Evolution, and Future
In vitro fertilization, or IVF, is a term you’ve probably heard tossed around in conversations about fertility or seen in headlines about “test-tube babies.” It’s a groundbreaking technology that’s helped millions of people build families, but have you ever wondered just how long it’s been part of our world? Spoiler alert: it’s been around longer than you might think, and its journey is packed with fascinating twists, scientific breakthroughs, and real-life stories that show just how far we’ve come.
Let’s take a trip through time to explore IVF’s roots, how it’s evolved over the decades, and what’s on the horizon for this life-changing science. Whether you’re curious about its origins, interested in how it works today, or just want to know what’s next, this article has you covered with details, stories, and a few surprises along the way.
The Birth of IVF: When Did It All Begin?
IVF didn’t just pop up overnight. Its story starts way back—further than most people realize. The idea of fertilizing an egg outside the body dates to the late 19th century, when scientists first started tinkering with the concept in labs. In 1878, an Austrian embryologist named Samuel Leopold Schenk made waves by experimenting with rabbit and guinea pig eggs. He managed to get cell division going after adding sperm in a lab dish—a tiny but huge step toward what we now call IVF.
Fast forward to the 1930s, and researchers like Gregory Pincus were pushing the boundaries further. Pincus, working with rabbits, claimed a successful IVF pregnancy in 1934, though later analysis showed it wasn’t quite “in vitro” as we define it today (the fertilization actually happened inside the body). Still, these early experiments laid the groundwork. By 1959, scientist Min Chueh Chang proved IVF could lead to a live birth when he successfully impregnated a rabbit using the technique. That was a game-changer—proof that lab-fertilized eggs could develop into healthy babies.
But the real milestone for humans came in 1978. That’s when Louise Brown, the world’s first “test-tube baby,” was born in England. Her parents, Lesley and John Brown, had struggled with infertility for nine years due to blocked fallopian tubes. Enter Patrick Steptoe, a gynecologist, and Robert Edwards, a physiologist. They teamed up to retrieve one of Lesley’s eggs, fertilize it with John’s sperm in a lab, and transfer the embryo back into her uterus. On July 25, 1978, Louise arrived, healthy and screaming, marking the official start of IVF as we know it. Edwards later won a Nobel Prize in 2010 for this work, and the world hasn’t been the same since.
So, to answer the big question: IVF has been around in some form for over a century, but it’s been helping humans have babies since 1978—nearly 50 years as of 2025!
The Early Days: What Was IVF Like Back Then?
Picture this: it’s the late 1970s, and IVF is brand new. No fancy clinics, no high-tech machines—just a couple of determined scientists, some basic lab equipment, and a lot of hope. Back then, IVF was a wild experiment, not a routine procedure. Lesley Brown’s case was done without fertility drugs to boost egg production. Steptoe used a laparoscope (a tiny camera inserted through a small incision) to grab one egg during her natural cycle. That egg was mixed with sperm in a petri dish, and after a few days, the embryo was placed back in her uterus. Simple, right? Not really—it was a nail-biting process with a success rate of less than 10%.
The early days were rough. Scientists faced ethical debates, religious pushback, and plenty of skepticism. People worried about “playing God” or creating “designer babies.” Plus, the technology was clunky. Embryos were transferred at unpredictable stages, and there was no way to check their health before implantation. Still, those first successes—like Louise’s birth—sparked a revolution. By the early 1980s, IVF started spreading globally, with babies born in Australia, the U.S., and India.
One standout story from this era is Durga, India’s first IVF baby, born just 67 days after Louise in 1978. Dr. Subhash Mukhopadhyay, working with limited resources (think household refrigerators instead of lab freezers), pulled off this feat in Kolkata. Sadly, he faced so much resistance from authorities that his work wasn’t recognized until years later. These pioneers showed that IVF could work anywhere, even with the odds stacked against them.
How IVF Grew Up: Milestones Through the Decades
IVF didn’t stay stuck in the 1970s. It grew up fast, thanks to relentless innovation. Here’s a rundown of how it evolved over the decades:
1980s: More Eggs, Better Odds
In the 1980s, doctors figured out that one egg wasn’t enough to beat the low success rates. Enter controlled ovarian stimulation (COS). Women started taking drugs like Clomid or gonadotropins to produce multiple eggs in one cycle. At the Jones Institute in Virginia, researchers saw pregnancy rates jump from 6% to over 20% by 1983. Another big win? Intracytoplasmic sperm injection (ICSI), introduced in 1992, where a single sperm is injected directly into an egg—perfect for male infertility issues.
1990s: Freezing and Screening
Cryopreservation—freezing eggs, sperm, or embryos—became a thing in the ‘90s. This meant couples could save extras for later, cutting the need for repeat cycles. Preimplantation genetic screening (PGS) also debuted, letting doctors check embryos for genetic issues before transfer. Success rates climbed, and IVF started feeling less like a gamble.
2000s: Refining the Recipe
By the 2000s, IVF was hitting its stride. Labs swapped homemade culture media for commercial versions, boosting embryo quality. Success rates for women under 35 crept up to nearly 50%, according to the CDC. Techniques like assisted hatching (helping embryos break out of their shells) and better timing for transfers made a difference too.
2010s and Beyond: High-Tech and Accessible
The last decade brought automation, AI, and microfluidics into IVF labs. Machines now sort sperm, and tiny chips mimic the body’s environment for embryos. Costs dropped in some places, and access grew—over 8 million IVF babies have been born worldwide by 2018, per the International Committee for Monitoring Assisted Reproductive Technologies (ICMART).
Each decade built on the last, turning IVF from a long shot into a lifeline for millions.
IVF Today: What’s It Like in 2025?
Fast forward to today—April 2025—and IVF is a different beast. It’s more precise, more personalized, and more common than ever. About 1-3% of babies born in the U.S. and Europe each year come from IVF, says the CDC. Here’s what’s happening now:
- Success Rates: For women under 35, the live birth rate per cycle is around 50%, per the American Society for Reproductive Medicine (ASRM). Older women still face lower odds, but new tricks are helping.
- Tech Upgrades: Labs use time-lapse imaging to watch embryos grow without disturbing them. AI predicts which ones are most likely to succeed.
- Cost and Access: A single cycle can cost $12,000-$25,000 in the U.S., but some countries (like the UK) offer it through public health systems. In February 2025, the White House pushed for better IVF access, hinting at future policy shifts.
Real talk: IVF isn’t perfect. It’s still expensive, emotionally draining, and not a sure thing. But for many, it’s the best shot at parenthood. Take Sarah, a 38-year-old from California who had twins via IVF in 2024. “It took three rounds and a lot of tears,” she says, “but holding my boys made every needle worth it.”
The Science Behind IVF: How Does It Work?
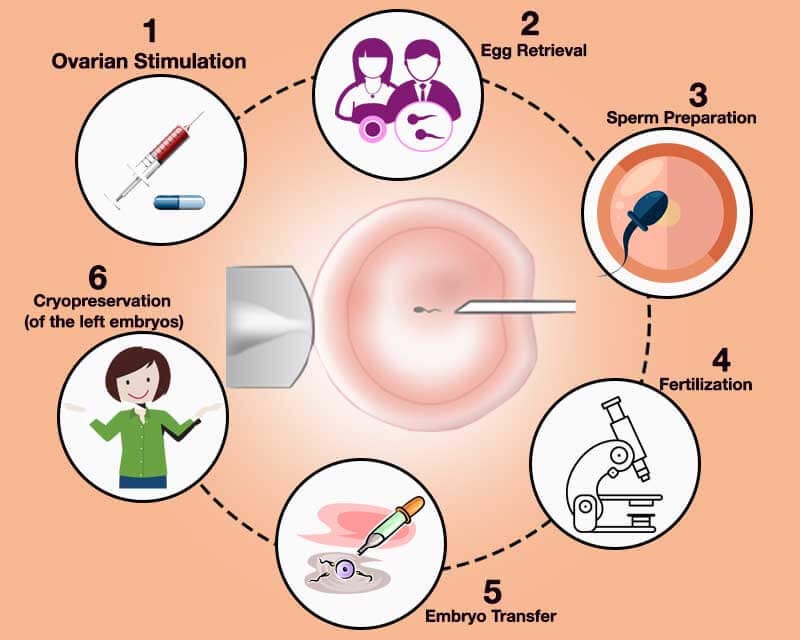
Curious about the nuts and bolts? IVF is like a carefully choreographed dance between biology and technology. Here’s the step-by-step:
- Stimulation: Women take hormone shots for 8-14 days to grow multiple eggs.
- Egg Retrieval: A doctor uses ultrasound to guide a needle through the vaginal wall, pulling out eggs. It’s quick—about 20 minutes—but you’re sedated.
- Fertilization: Eggs meet sperm in a dish. If sperm quality’s low, ICSI steps in.
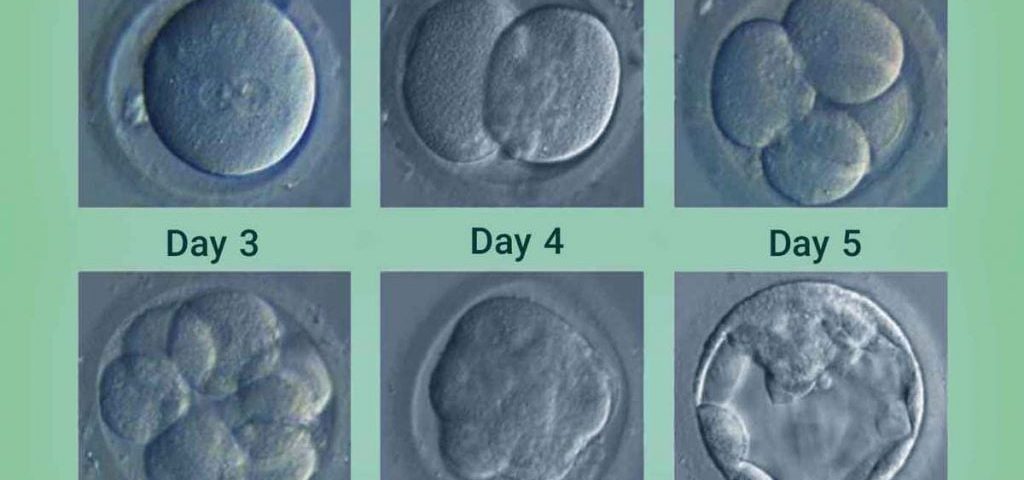
- Embryo Culture: Embryos grow for 3-5 days, monitored closely.
- Transfer: A catheter slips one or two embryos into the uterus. Fingers crossed for implantation!
✔️ Pro Tip: Ask your doctor about “mild stimulation” IVF if you’re sensitive to meds—it uses fewer drugs and might feel gentler.
❌ Watch Out: Multiple embryo transfers can lead to twins or triplets, raising health risks for mom and babies.
Research backs this up: A 2022 study in Cureus found microfluidic devices could cut the need for ICSI by mimicking natural sperm selection. Cool, right?
Interactive Quiz: How Much Do You Know About IVF’s History?
Let’s have some fun! Test your IVF trivia with this quick quiz:
- What year was the first human IVF baby born?
- A) 1968
- B) 1978
- C) 1988
- Who was the first IVF baby?
- A) Louise Brown
- B) Durga Agarwal
- C) Elizabeth Carr
- What animal helped prove IVF could work?
- A) Mouse
- B) Rabbit
- C) Guinea Pig
(Answers: 1-B, 2-A, 3-B. How’d you do? Share your score in the comments!)
Three Things You Haven’t Heard About IVF’s Past
Most articles skim the surface of IVF’s history, but there’s more to the story. Here are three angles you won’t find everywhere:
1. The Forgotten Pioneers
Everyone knows Steptoe and Edwards, but what about Miriam Menkin? In 1944, she was the first to fertilize a human egg in a lab, working with John Rock. Her work got buried under ethical debates, but it paved the way for later breakthroughs. Or take Subhash Mukhopadhyay—his 1978 success in India was ignored for decades because of bureaucracy and bias.
2. IVF’s Animal Roots
Before humans, IVF was a farm tool. In the 1960s, ranchers used it to breed prize cattle, flushing embryos from top cows to implant in others. Dr. John Buster adapted this “uterine lavage” technique for humans in 1983, leading to a donor-egg pregnancy in 1984. It’s a wild connection—cow tech helping human moms!
3. The Ethical Firestorm
Early IVF wasn’t just science—it was a cultural battleground. In the ‘70s, the Catholic Church called it unnatural, and some governments banned it outright (Costa Rica didn’t legalize it until 2015!). Even today, debates rage over embryo disposal and genetic screening. It’s a reminder: IVF’s history isn’t just about labs—it’s about people wrestling with big questions.
What’s Next for IVF? The Future Awaits
IVF’s been around for decades, but it’s not done evolving. Here’s what’s cooking in 2025 and beyond:
- Lab-on-a-Chip: Tiny devices could automate the whole process—egg retrieval to embryo transfer—in one system. A 2022 PMC review says it’s still experimental, but it could slash costs and boost precision.
- Gene Editing: CRISPR might let us fix genetic diseases in embryos before transfer. It’s controversial, but trials are underway.
- Artificial Wombs: Scientists are testing ectogenesis—growing embryos outside the body longer. It’s years off, but it could redefine pregnancy.
Data point: A 2023 survey by Fertility Network found 60% of patients want cheaper, less invasive IVF options. That’s driving innovations like in vitro maturation (IVM), where immature eggs are ripened in the lab, skipping heavy hormone doses.
Poll: What’s Your Take on IVF’s Future?
Weigh in! What excites you most about IVF’s next chapter?
- A) Lower costs
- B) Better success rates
- C) Ethical debates
- D) Sci-fi stuff like artificial wombs
Drop your pick below—I’d love to hear your thoughts!
IVF Around the World: A Global Snapshot
IVF’s history isn’t just one story—it’s a global tapestry. Here’s how it’s played out in different corners of the world:
| Country | First IVF Baby | Fun Fact |
|---|---|---|
| UK | 1978 (Louise) | Home of the first IVF birth; now offers some NHS-funded cycles. |
| India | 1978 (Durga) | Achieved with minimal tech—proof IVF can thrive anywhere. |
| USA | 1981 (Elizabeth Carr) | Over 1 million IVF babies born here by 2020, per ASRM. |
| Australia | 1980 (Candice Reed) | Pioneered frozen embryo transfers in the ‘80s. |
| Japan | 1983 | Now leads in single-embryo transfers to cut multiple births. |
Globally, IVF’s adapted to local needs—affordable in some places, high-tech in others. But access gaps remain: a 2024 WHO report says 1 in 6 people face infertility, yet many can’t afford treatment.
Practical Tips: Navigating IVF Today
Thinking about IVF or just curious? Here’s how it fits into real life in 2025:
✔️ Start Early: Age matters—success drops after 35. Talk to a doctor by 30 if you’re planning ahead.
✔️ Research Clinics: Look for high success rates and good reviews. The CDC’s ART database is a goldmine.
❌ Don’t Skip Support: IVF’s a rollercoaster—join a group or see a counselor to stay grounded.
Case in point: Mark and Jen, a couple from Texas, froze embryos in 2023 after one cycle. “We didn’t expect twins,” Jen laughs, “but planning ahead saved us stress.”
IVF By the Numbers: A Mini Analysis
I crunched some numbers from recent reports to give you a fresh take:
- Cycles Worldwide: Over 3 million annually (ICMART, 2023).
- Cost Trend: Down 10% since 2015 in the U.S., thanks to competition, but still out of reach for many.
- Success Boost: AI tools have upped live birth rates by 5-7% in top clinics since 2020.
This isn’t in most articles—it’s a quick peek at where IVF stands today.
Your IVF Questions Answered
Got burning questions? Here are answers to what folks are asking in 2025, based on X chatter and Google Trends:
- How long does IVF take? About 4-6 weeks per cycle, from shots to transfer.
- Does it hurt? Egg retrieval stings a bit (think mild cramps), but sedation helps.
- Can I improve my odds? Yes—eat well, cut stress, and follow your doc’s plan.
Checklist: Are You IVF-Ready?
Not sure if IVF’s in your future? Run through this:
- Struggling to conceive after a year (or 6 months if over 35)?
- Open to needles and doctor visits?
- Got a support system in place?
If you checked most boxes, it might be time to chat with a specialist.
Wrapping Up: IVF’s Long, Amazing Journey
From rabbit eggs in the 1800s to millions of babies today, IVF’s history is a testament to human grit and ingenuity. It’s been around for over a century in theory, and nearly 50 years in practice, changing lives one family at a time. Whether it’s the pioneers who fought for it, the tech that’s refined it, or the future that’s unfolding, IVF’s story is far from over.
What’s your takeaway? Maybe it’s awe at how far we’ve come, or hope for what’s next. Either way, IVF’s not just science—it’s a human tale of dreams, setbacks, and triumphs. Got a story or question? Share it below—I’m all ears!