How Many Children Were Conceived Using IVF in 2023?
April 20, 2025
What Does Lupron Do for IVF?
April 21, 2025How Many Births Are From IVF? Exploring the Numbers, Trends, and Stories Behind the Science
In today’s world, starting a family isn’t always as simple as it sounds. For millions of people, in vitro fertilization (IVF) has become a game-changer, turning dreams of parenthood into reality. But just how many babies are born thanks to this incredible technology? If you’ve ever wondered about the numbers—or what IVF really means for families—this article is for you. We’re diving deep into the stats, the science, and the stories, plus some surprising insights you won’t find everywhere else. Grab a comfy seat, and let’s explore this together!
What Is IVF, and Why Does It Matter?
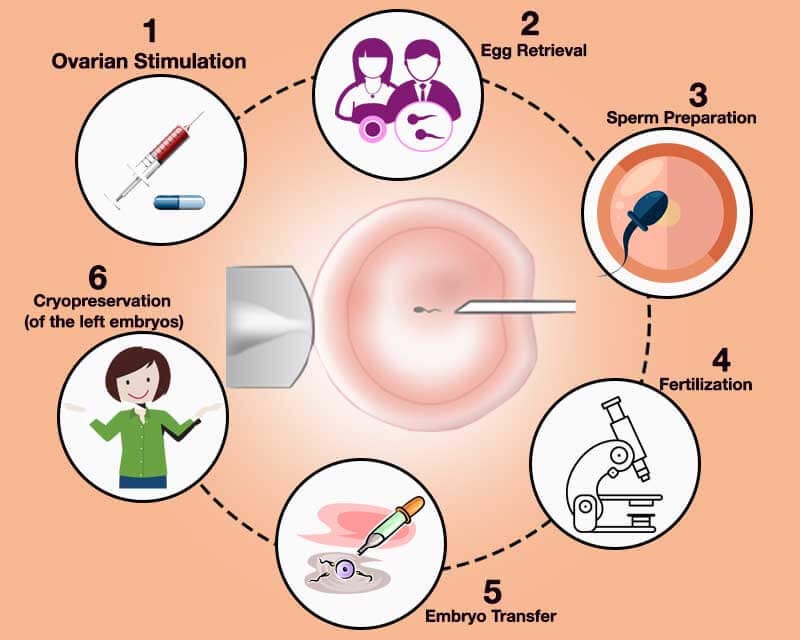
IVF stands for in vitro fertilization, a process where doctors combine an egg and sperm outside the body in a lab. Once an embryo forms, it’s placed into the uterus, hoping it grows into a healthy baby. It’s like giving nature a little nudge when things don’t work out on their own. This method has been around since 1978, when the first IVF baby, Louise Brown, was born in England. Since then, it’s helped countless families overcome infertility, medical challenges, or even build families in unique ways—like for same-sex couples or single parents.
Why does it matter? Because infertility affects about 1 in 7 couples in the U.S. alone, and IVF offers hope where there once was none. It’s not just a medical procedure—it’s a lifeline for people longing to hold their own child. So, how big of an impact does it really have? Let’s look at the numbers.
The Big Picture: How Many Babies Are Born Through IVF?
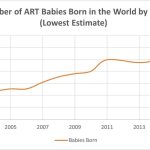
Every year, IVF plays a huge role in bringing new life into the world. In the United States, about 97,000 babies were born from assisted reproductive technologies (ART) like IVF in 2021, according to the latest data from the Centers for Disease Control and Prevention (CDC). That’s roughly 1 out of every 42 babies born nationwide—or about 2.3% of all births. To put that in perspective, imagine filling a giant stadium with newborns—all thanks to IVF!
Globally, the numbers are even more jaw-dropping. Since Louise Brown’s birth, experts estimate that over 8 million babies have been born worldwide through IVF and other ART methods. Some studies even suggest the number could be closer to 10 million by now, given how fast the technology is growing. In countries like Denmark, where IVF is widely available and often covered by insurance, it accounts for over 5% of all births. That’s a lot of little miracles!
But here’s something wild to think about: those numbers are just the tip of the iceberg. For every successful IVF birth, there are many more cycles that don’t work out. So, the real story isn’t just about the babies born—it’s about the effort, hope, and science behind every attempt.
Breaking Down the U.S. Numbers: A Closer Look
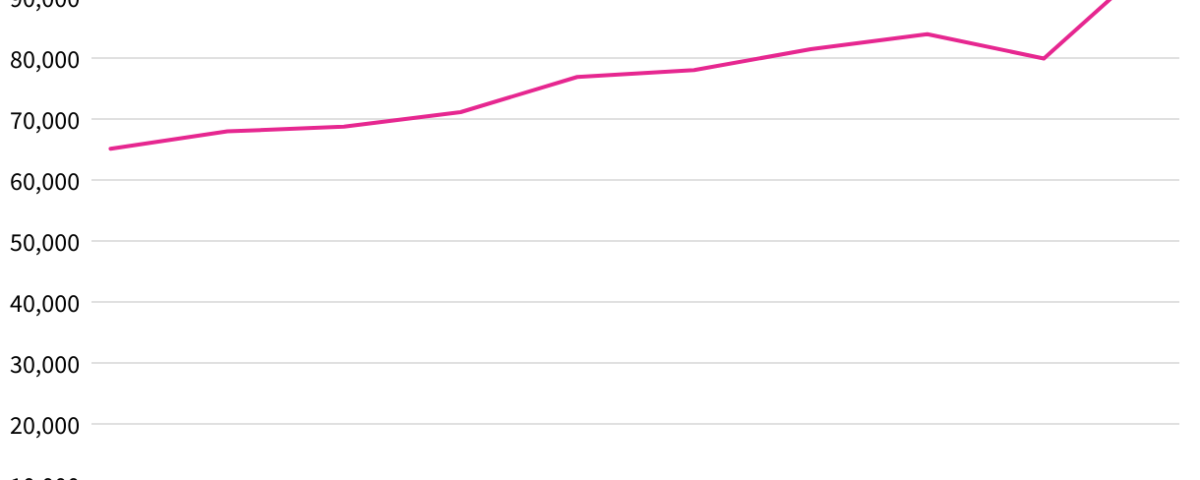
Let’s zoom in on the U.S. for a second. The CDC tracks IVF through its National ART Surveillance System, and the 2021 report gives us a clear snapshot. Out of about 3.7 million total births that year, 97,128 came from ART procedures—99% of which were IVF. That’s a big jump from a decade ago, when the number was closer to 65,000 in 2012. In fact, the use of IVF has more than doubled since the early 2000s!
What’s driving this growth? A few things:
- More Awareness: People know about IVF now more than ever, thanks to celebrities sharing their stories and better education from doctors.
- Delayed Parenthood: Women are having kids later—sometimes in their 30s or 40s—when natural fertility drops, making IVF a go-to option.
- Tech Advances: New techniques, like freezing embryos or testing them for genetic issues, have made IVF more successful.
But not every state sees the same IVF action. In Massachusetts, where insurance often covers it, 4.5% of babies are born via ART. Compare that to New Mexico, where it’s just 0.5%. Access, cost, and local clinics make a huge difference.
Fun Fact: IVF’s Growing Footprint
If you added up all the U.S. citizens alive today who were born through IVF, you’d get about 3.6 million people. That’s more than the population of Chicago! It’s a reminder of how this technology has quietly shaped our society.
How Does IVF Stack Up Globally?
The U.S. isn’t the only place where IVF is making waves. Around the world, the numbers tell an even bigger story. In Europe, countries like Spain and the UK are IVF powerhouses. The Human Fertilisation and Embryology Authority (HFEA) in the UK reported that in 2022, about 77,000 IVF cycles led to thousands of births—pushing the UK’s total IVF babies past 390,000 since 1991.
In Asia, China’s IVF scene is booming too. With a population of over 1.4 billion, even a small percentage of IVF births adds up fast. Experts estimate that 1.7% of Chinese babies—about 300,000 a year—are now born through ART. And in Australia, the rate’s at 4.1%, showing how common it’s become in some places.
What’s cool is how these numbers shift depending on where you look. In Japan, where people also delay having kids, IVF is on the rise, but costs and cultural attitudes keep it lower than in Europe. Meanwhile, in less wealthy countries, access is still limited, so the global total is skewed toward richer nations.
Why Aren’t These Numbers Higher? The Success Rate Reality
Here’s a question you might be asking: If IVF is so great, why isn’t it behind more births? The answer lies in success rates—and they’re not as high as you might hope. On average, only about 25-30% of IVF cycles result in a live birth, depending on factors like age, health, and the clinic’s expertise.
For women under 35 using their own eggs, the success rate per embryo transfer is around 40-50%. But for women over 40, it drops to about 24%. If donor eggs are used, the odds jump back up to 50% or more, no matter the mom’s age. That’s why some families try multiple rounds—sometimes 3, 5, or even more—before they get a baby.
Quick Stats Snapshot
| Age Group | Success Rate (Own Eggs) | Success Rate (Donor Eggs) |
|---|---|---|
| Under 35 | 40-50% | 50-55% |
| 35-37 | 35-40% | 50-55% |
| 38-40 | 25-30% | 50-55% |
| Over 40 | 10-24% | 42-53% |
This gap explains why the number of IVF births isn’t sky-high. For every baby born, there are tons of embryos that don’t make it—either because they don’t implant, aren’t viable, or get frozen for later. It’s a tough reality, but it’s also why every IVF birth feels like a victory.
The Hidden Numbers: Embryos That Don’t Become Babies
One thing you won’t see in most articles is what happens to all the embryos created during IVF that don’t lead to births. This is a big deal—and a bit of an emotional rollercoaster for families. In a typical IVF cycle, doctors might create 5-10 embryos, but only 1 or 2 get transferred right away. The rest? They’re either frozen, discarded if they’re not healthy, or donated.
Studies suggest that for every live birth, 3-8 embryos never get a chance to implant. That means millions of embryos worldwide are part of the IVF story but don’t end up as babies. Some families freeze them for future tries—about 1 million embryos are currently stored in the U.S. alone! Others face tough choices about what to do with extras, like donating them to research or other couples.
This part of IVF doesn’t get much airtime, but it’s a huge piece of the puzzle. It shows how much effort goes into each success—and why the numbers we see are just the start.
What’s Driving IVF’s Popularity Today?
IVF isn’t just growing because of infertility. People are using it for all kinds of reasons, and that’s pushing the numbers up. Here’s what’s fueling the trend:
- Later Parenthood: More women are waiting until their 30s or 40s to have kids, when fertility naturally dips. In the U.S., the average age of first-time moms is now 27, up from 21 in 1970. IVF steps in when time’s not on their side.
- Family Diversity: Single parents and same-sex couples are turning to IVF with donor eggs, sperm, or surrogates. In 2022, the UK saw a spike in IVF for female couples, making up 7% of cycles.
- Fertility Preservation: People freeze eggs or embryos before cancer treatments or just to plan ahead. It’s like a backup plan for future babies.
- Genetic Screening: IVF lets parents test embryos for conditions like Down syndrome before pregnancy, which appeals to some.
Social media’s buzzing about this too. Posts on X show folks celebrating IVF successes, but also venting about costs and access. It’s a hot topic—and it’s only getting hotter.
Interactive Quiz: What’s Your IVF IQ?
Think you know IVF? Test yourself!
- What year was the first IVF baby born?
- A) 1968 B) 1978 C) 1988
- About how many U.S. babies are born via IVF each year?
- A) 50,000 B) 97,000 C) 150,000
- What’s the biggest reason people use IVF?
- A) Infertility B) Fun C) Curiosity
(Answers: 1-B, 2-B, 3-A. How’d you do?)
- A) Infertility B) Fun C) Curiosity
The Cost Factor: Why IVF Isn’t Everywhere
If IVF is so amazing, why isn’t every baby an IVF baby? Money’s a big hurdle. One cycle can cost $12,000 to $25,000 in the U.S., and most insurance plans don’t cover it. That’s a car—or a year of college! Families often save up, take loans, or even crowdfund to make it happen.
Compare that to places like the UK, where the National Health Service (NHS) funds some cycles, or Denmark, where it’s free for many. No wonder their IVF rates are higher! In the U.S., only 19 states mandate some insurance coverage, and even then, it’s spotty. Posts on X often rant about this—people want change, and they’re loud about it.
Tips to Make IVF More Affordable
✔️ Shop Around: Clinic prices vary—some offer payment plans.
✔️ Look for Grants: Groups like Baby Quest give money to families.
✔️ Consider Mini-IVF: It uses fewer drugs, cutting costs by thousands.
❌ Don’t Skip Research: Cheaper isn’t always better—check success rates!
New Tech Changing the Game
IVF isn’t stuck in the past—it’s evolving fast. Here are three breakthroughs you might not have heard about:
1. AI in the Lab
Artificial intelligence is helping doctors pick the best embryos. A 2023 study found AI boosted success rates by 20% in some clinics. It’s like having a super-smart assistant who never sleeps!
2. At-Home Monitoring
Portable ultrasound devices and saliva tests for hormone levels are making IVF less of a clinic slog. Imagine checking your progress from your couch—some patients already are.
3. Lab-Grown Eggs
Scientists are working on turning skin cells into eggs or sperm. It’s still experimental, but it could mean no more donor shortages. A 2022 trial in mice worked—humans might be next.
These advances could push IVF births even higher in the future. They’re cutting costs, upping success, and making it easier for more people to try.
Real Stories: The Faces Behind the Numbers
Numbers are great, but stories hit home. Take Sarah, a 38-year-old teacher from Ohio. After three years of trying naturally, she and her husband turned to IVF. Two cycles, $30,000, and a lot of tears later, their son Ethan was born in 2023. “It was worth every penny,” she says. “He’s our world.”
Then there’s James and Michael, a couple from California. They used IVF with a surrogate and donor eggs to welcome twins in 2021. “We never thought we’d be dads,” James says. “IVF made it real.”
These aren’t just stats—they’re lives changed. And there are millions more like them.
IVF’s Future: Where Are We Headed?
So, how many births will be from IVF in 10 or 20 years? Experts predict the numbers will climb—maybe to 5% or more in the U.S.—as tech improves and costs drop. A 2022 study even suggested that by 2100, ART could account for 3% of the world’s population, or 400 million people!
What could make this happen?
- Better Access: If insurance or governments step up, more families could afford it.
- Cultural Shifts: As stigma fades, more people might choose IVF early on.
- Climate and Health: Some researchers think pollution and stress are hurting fertility, pushing more toward IVF.
Poll Time: What Do You Think?
Should health insurance cover IVF?
- Yes, it’s a medical need!
- No, it’s too expensive for everyone.
- Not sure—depends on the cost.
Drop your vote in the comments!
Three Things You Haven’t Heard About IVF
Most articles stick to the basics, but here are three angles you won’t find everywhere:
1. IVF’s Environmental Footprint
Labs use tons of energy and plastic—think petri dishes and freezers. A 2023 analysis estimated that one IVF cycle produces as much carbon as driving 100 miles. Clinics are starting to go green, but it’s a hidden cost of those 97,000 babies.
2. The Mental Health Toll
Everyone talks about success, but what about the 70% of cycles that fail? Studies show IVF patients face higher rates of anxiety and depression—sometimes lasting years. Support groups and therapy are key, yet often overlooked.
3. IVF’s Role in Population Growth
In places like Japan, where birth rates are tanking, IVF could be a fix. A 2024 report suggested it might add 1% to their population by 2050 if funded right. It’s not just about individuals—it’s about whole countries!
Practical Tips for Anyone Considering IVF
Thinking about IVF? Here’s a step-by-step guide to get started:
- Talk to a Doctor: Find a fertility specialist and ask about your odds.
- Check Your Wallet: Look at costs and insurance—plan for at least $15,000.
- Boost Your Health: Eat well, sleep lots, and cut stress—it helps eggs and sperm.
- Build a Support Crew: Friends, family, or a counselor can keep you sane.
- Ask Questions: What’s the clinic’s success rate? How many cycles might it take?
A Little Math: My Own IVF Birth Estimate
I crunched some numbers for fun. If the U.S. has 97,000 IVF births a year and that grows by 5% annually (a reasonable guess based on past trends), we’d hit 150,000 by 2030. Globally, if the 8 million total rises at 3% a year, we could see 12 million IVF babies by 2035. It’s not official, but it shows how fast this could grow!
Wrapping It Up: IVF’s Amazing Impact
So, how many births are from IVF? Right now, it’s about 97,000 a year in the U.S. and millions worldwide, with a legacy of over 8 million babies since 1978. But it’s more than numbers—it’s hope, science, and families made whole. From AI picking embryos to parents fighting for every chance, IVF is rewriting what’s possible.
What’s your take? Have you or someone you know tried IVF? Share your story below—I’d love to hear it. And if you’re curious about anything else, just ask. This journey’s too big to cover in one go, but we’ve got a great start!