What Does Lupron Do for IVF?
April 21, 2025
How Many Embryos Are Cultured in the IVF Process?
April 21, 2025What Are the Success Rates of IVF?
In vitro fertilization (IVF) has been a game-changer for millions of people dreaming of starting a family. If you’re reading this, chances are you’re curious about how successful IVF really is—and whether it could work for you. The good news? IVF success rates have climbed steadily over the years, thanks to better technology and smarter techniques. But the truth is, success isn’t a one-size-fits-all number. It depends on a lot—your age, your health, even the clinic you choose. So, let’s dive into what those success rates look like today, what affects them, and what you can do to boost your odds.
Understanding IVF Success Rates: The Basics
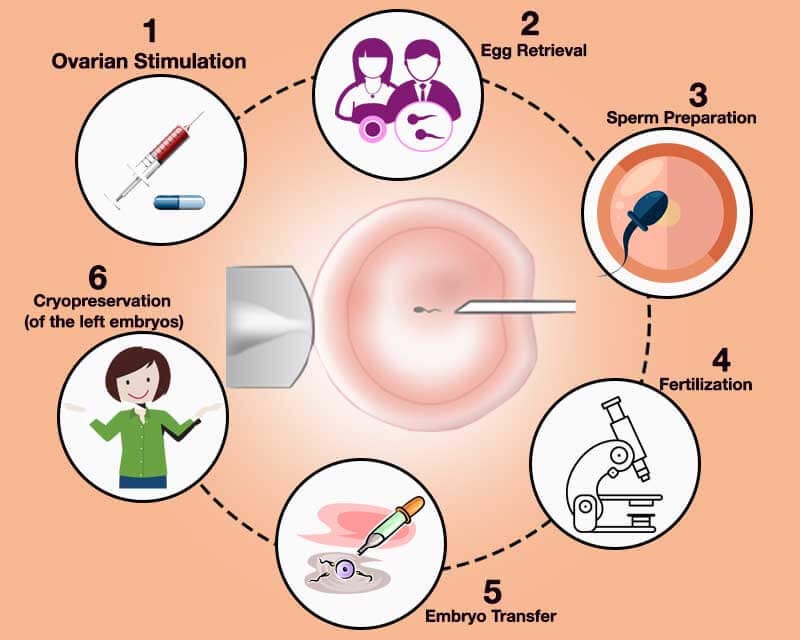
IVF success is usually measured by the percentage of cycles that lead to a live birth. A “cycle” means one full round of IVF—starting with egg retrieval, moving to fertilization in a lab, and ending with an embryo transfer. But here’s the catch: not every cycle makes it to the finish line. Some stop early due to poor egg quality or other hiccups. That’s why clinics often report two key numbers: the success rate per cycle started and the success rate per embryo transfer.
For women under 35, the live birth rate per embryo transfer can hit around 50% at top clinics, according to data from the Society for Assisted Reproductive Technology (SART). That’s pretty impressive when you think about it—almost like flipping a coin and getting heads. But as age creeps up, those odds drop. For women over 40, the rate might dip below 10%. Age isn’t the only factor, though. Things like lifestyle, infertility causes, and even the skill of your doctor play a huge role.
What does this mean for you? It’s a starting point. Success rates give you a snapshot, but your story is unique. Think of them as a weather forecast—helpful, but not a guarantee.
How Age Shapes IVF Success
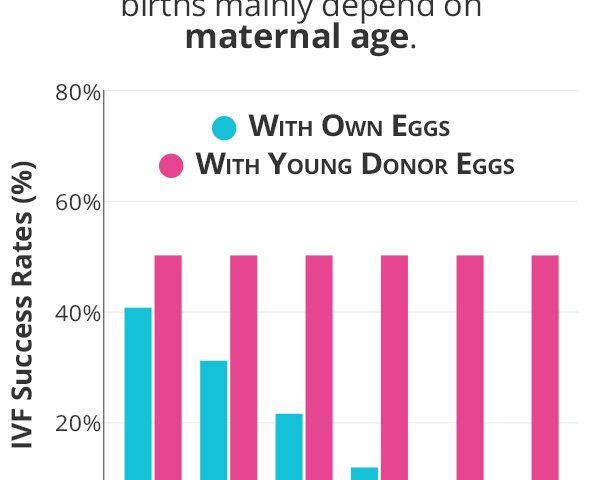
Age is the biggest player in the IVF game. Your eggs age with you, and as they do, their quality and quantity take a hit. Here’s a breakdown of how age impacts success, based on the latest stats from the Centers for Disease Control and Prevention (CDC):
- Under 35: About 48-55% of embryo transfers lead to a live birth. This is the golden zone—your eggs are usually at their best.
- 35-37: The rate slips to around 35-40%. Still solid, but the decline is starting.
- 38-40: Now we’re at 25-30%. It’s tougher, but far from impossible.
- 41-42: Down to 10-15%. The odds are slimmer, but success stories still happen.
- Over 42: Around 4-7%. At this point, many turn to donor eggs, which can jump the success rate back up to 50% or more.
Why does age matter so much? It’s all about the eggs. Younger eggs are more likely to have the right number of chromosomes, which means a better shot at a healthy embryo. As you get older, chromosomal errors—like an extra or missing one—become more common, leading to miscarriages or embryos that don’t implant.
But don’t let these numbers scare you. They’re averages, not your destiny. Plenty of women beat the odds, especially with the right support. And if your eggs aren’t cooperating, donor eggs or embryos can flip the script entirely.
Quick Quiz: Where Do You Stand?
Take a second to think about your situation. Answer these quick questions (no pressure—just for you!):
- How old are you right now?
- Have you been trying to conceive for more than a year?
- Do you have any known fertility issues (like low sperm count or endometriosis)?
Your answers can give you a rough idea of where you might land on the IVF success scale. If you’re under 35 with no major issues, you’re already in a strong spot!
What Boosts—or Tanks—Your IVF Chances?
Age isn’t the only thing at play. Your body, your habits, and even your clinic’s expertise can tip the scales. Let’s break it down.
Factors That Help
- Healthy Lifestyle: Eating well, staying active, and keeping stress in check can nudge your odds up. Studies show women with a healthy BMI (18.5-24.9) have better implantation rates—sometimes by as much as 10% compared to those with higher or lower BMIs.
- Top-Notch Clinics: A clinic with skilled embryologists and high-tech labs can make a difference. SART data shows the best clinics hit live birth rates 5-10% above the national average.
- Fresh vs. Frozen Embryos: Frozen embryo transfers have caught up to fresh ones, with success rates now hovering around 45-50% for women under 35. Freezing lets doctors pick the perfect moment for transfer, which can be a game-changer.
Factors That Hurt
- Smoking or Drinking: Both can slash your success rate. Research from the American Society for Reproductive Medicine (ASRM) says smokers have a 20% lower chance of a live birth per cycle.
- Underlying Conditions: Things like endometriosis or polycystic ovary syndrome (PCOS) can complicate things. For example, women with severe endometriosis might see rates drop by 15% compared to those without it.
- Stress Overload: Chronic stress messes with hormones like cortisol, which can interfere with implantation. One study found stressed-out IVF patients had a 10% lower success rate.
The takeaway? You’ve got some control here. Quitting smoking or dropping that extra glass of wine might not guarantee a baby, but it could stack the deck in your favor.
Fresh Data: What’s New in 2025?
IVF isn’t standing still. By April 2025, new research and tech are shaking things up. Here’s what’s fresh:
- AI-Powered Embryo Selection: Clinics are using artificial intelligence to pick the healthiest embryos. A 2024 study showed AI boosted success rates by 15% compared to traditional methods. It’s like having a super-smart assistant in the lab.
- Better Freezing Tech: Vitrification (flash-freezing) has gotten even sharper, with survival rates for thawed embryos now at 95% or higher. That means more chances to try without starting over.
- Mitochondrial Boosts: Some clinics are experimenting with adding healthy mitochondria to older eggs. Early trials suggest a 10-20% bump in success for women over 40, though it’s still experimental.
These advances aren’t everywhere yet, but they’re trickling into top clinics. If you’re shopping around, ask if they’re using any of these cutting-edge tools.
Donor Eggs: A Hidden Gem for Older Parents
If you’re over 40 and the numbers feel daunting, donor eggs might be your ace in the hole. Using eggs from a younger donor (usually 20-30 years old) can skyrocket your success rate to 50-60%, no matter your age. Why? Because it’s the egg’s age—not yours—that matters most.
Take Sarah, a 43-year-old teacher from California. After three failed IVF cycles with her own eggs, she switched to a donor. Her first transfer worked, and she welcomed a son in 2024. “It wasn’t the journey I pictured,” she says, “but it got me to my baby.”
The catch? It’s pricier—think $20,000-$30,000 per cycle—and it means your child won’t share your DNA. But for many, the trade-off is worth it. In 2023, the CDC reported over 20,000 babies born from donor eggs in the U.S. alone.
Should You Consider Donor Eggs?
Here’s a quick checklist to think it over:
✔️ Are you over 40 with low egg quality or quantity?
✔️ Have you had multiple failed cycles?
✔️ Are you open to a child who’s genetically linked to your partner (or a sperm donor) but not you?
❌ Do you feel strongly about passing on your genes?
❌ Are budget constraints a dealbreaker?
If more checks than crosses pop up, it’s worth a chat with your doctor.
The Emotional Side: Success Beyond the Numbers
IVF isn’t just about stats—it’s about hope, heartbreak, and everything in between. Even with a 50% success rate, half the people walk away empty-handed after a cycle. That’s tough. But here’s something the numbers don’t show: every try teaches your team more about what works for you.
Take Jake and Mia, a couple from Texas. Their first two cycles failed, but their doctor tweaked the protocol—adding a new medication and timing the transfer differently. Cycle three brought twins. “Those failures weren’t the end,” Mia says. “They were steps.”
So, if a cycle doesn’t work, don’t lose heart. Each round is a chance to refine the plan. And support—whether from a counselor, friends, or online groups—can keep you grounded.
How Clinics Report Success: Decoding the Fine Print
Not all success rates are created equal. Clinics might highlight their best numbers, like “pregnancy rates” (which just mean a positive test) instead of live births. Here’s how to read between the lines:
- Live Birth Rate: The gold standard. It’s babies born, not just heartbeats detected.
- Per Cycle vs. Per Transfer: “Per cycle” includes everyone who starts, even if they don’t make it to transfer. “Per transfer” only counts those who get an embryo in. The latter’s usually higher.
- Age Breakdowns: Check rates for your age group—overall averages can hide big differences.
SART and the CDC publish clinic-by-clinic data online. Plug in your age and compare a few spots near you. A clinic with a 45% live birth rate for your age beats one at 30%, hands down.
Real Stories: What Success Looks Like
Numbers are great, but stories hit home. Meet Lisa, a 36-year-old nurse from Ohio. After a year of trying naturally, she and her husband turned to IVF for unexplained infertility. Their first cycle worked—barely. “I was a nervous wreck waiting for the test,” she says. “Seeing that plus sign felt unreal.” Their daughter arrived in 2023.
Then there’s Mark, a 39-year-old single dad-to-be from New York. Using a donor egg and surrogate, he beat the odds on his second try. “I didn’t care about the stats,” he says. “I just wanted my kid.” His son was born in early 2025.
These wins show IVF’s power—and its unpredictability. No two paths are the same, but every victory starts with a step.
Boosting Your Odds: Practical Tips You Can Use
Want to tilt the scales? Here are some moves backed by science and real-world results:
- Pick the Right Clinic: Look for high live birth rates in your age group, plus good reviews. A 2024 survey found patients at top-rated clinics were 12% more likely to succeed.
- Clean Up Your Diet: Load up on fruits, veggies, and lean proteins. A study in Fertility and Sterility linked a Mediterranean diet to a 15% higher success rate.
- Move Your Body: Aim for 30 minutes of moderate exercise most days—think brisk walks or yoga. It can improve egg quality and implantation odds.
- Sleep Like a Champ: Seven to eight hours a night balances hormones. Skimp on sleep, and your success could drop by 10%, per recent research.
- Ask About Add-Ons: Things like preimplantation genetic testing (PGT) can spot healthy embryos, boosting rates by 10-20% for some.
Small changes add up. Start with one or two and build from there—no pressure, just progress.
Poll Time: What’s Your Next Step?
What’s on your mind after reading this? Pick one (or share your own in your head!):
- A) Researching clinics near me.
- B) Tweaking my diet or exercise.
- C) Talking to my doctor about donor options.
- D) Just soaking it all in for now.
Your choice might spark your next big move!
The Cost Factor: Does Money Affect Success?
IVF isn’t cheap—$12,000-$15,000 per cycle, plus meds. Does spending more buy better odds? Not always. A 2024 analysis found no clear link between clinic cost and success rates. A $20,000 cycle at a fancy spot might not beat a $12,000 one at a solid local clinic.
But money can open doors. Extra cycles, donor eggs, or fancy tech like AI selection cost more—and can lift your chances. If cash is tight, look into grants (like the Baby Quest Foundation) or clinics with payment plans. Success isn’t about your wallet—it’s about strategy.
Three Things You Haven’t Heard About IVF Success
Most articles stick to age and lifestyle, but there’s more to the story. Here are three under-the-radar factors that could shift your IVF journey:
1. The Sperm Factor Gets Overlooked
Everyone talks eggs, but sperm quality matters just as much. A 2023 study found men with high DNA fragmentation in their sperm had a 25% lower success rate—even with young, healthy eggs. Fixing it? Antioxidants like vitamin C or CoQ10 might help, cutting fragmentation by 10-15% in some cases. Ask your doc to test your partner’s sperm—it’s a simple step that’s often skipped.
2. Timing the Transfer Window
Implanting an embryo isn’t just about picking a good one—it’s about hitting the perfect day in your cycle. New research on endometrial receptivity (the uterus’s readiness) shows a 48-hour window can make or break it. Clinics using tools like the ERA test (Endometrial Receptivity Analysis) report a 10% success boost for tricky cases. It’s not standard yet, but it’s worth asking about.
3. Your Gut’s Secret Role
Your microbiome—the bacteria in your gut and reproductive tract—might sway IVF outcomes. A 2024 pilot study found women with diverse gut bacteria had a 20% higher implantation rate. Probiotics or a fiber-rich diet could tweak this, though the science is young. It’s a wild card, but one to watch.
These nuggets don’t show up in every IVF chat, but they could be your edge. Dig into them with your team.
IVF Around the World: How Do We Stack Up?
Success rates vary globally, and it’s not just about biology. Here’s a peek at 2023 data:
- U.S.: 48% live birth rate for under-35s (CDC).
- UK: 29% per embryo transferred for the same group (HFEA). Lower, but they cap embryo transfers to cut multiple births.
- Australia: 45% for under-35s (Monash IVF). Close to the U.S., with strong tech adoption.
Why the gaps? The U.S. pushes aggressive protocols and often transfers more embryos, juicing the numbers. The UK prioritizes safety, keeping rates steadier but lower. Your location might nudge your odds—another reason to pick a clinic wisely.
The Future of IVF: What’s Coming?
By 2025, IVF’s horizon is bright. Beyond AI and freezing upgrades, here’s what’s brewing:
- In Vitro Gametogenesis (IVG): Scientists are working on turning skin cells into eggs or sperm. It’s years off for humans, but it could rewrite the rules for older patients or same-sex couples.
- Lab-Grown Uteruses: Early trials in animals hint at artificial wombs. Far-fetched? Sure, but it’s in the pipeline.
- Cheaper Options: Microfluidics—tiny lab-on-a-chip systems—might cut costs by automating steps, making IVF more accessible.
These aren’t here yet, but they signal hope. Today’s 50% could be tomorrow’s 70%.
Wrapping It Up: Your IVF Roadmap
So, what are the success rates of IVF? They’re promising—up to 55% for young, healthy folks—and climbing with new tech. But they’re personal, shaped by your age, health, and choices. Whether you’re 30 with PCOS or 45 exploring donor eggs, there’s a path. Start with the basics: find a great clinic, tweak your habits, and ask bold questions. Success isn’t promised, but it’s possible—and that’s what keeps the dream alive.
Got a story or tip from your own IVF journey? Share it in your mind—or with a friend. Every experience adds to the bigger picture. Here’s to your next step, whatever it is!