How Many Times Can You Do IVF in a Year?
April 21, 2025
What Did the IVF Bill Contain? A Deep Dive into Its Purpose, Provisions, and Impact
April 21, 2025What Is the IVF Procedure? Your Complete Guide to In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might have heard tossed around in conversations about starting a family, especially when things don’t go as planned. It’s a fertility treatment that’s helped millions of people worldwide become parents, and it’s more common than you might think—over 10 million babies have been born through IVF since it first made headlines in 1978. But what exactly is it? How does it work? And what should you expect if you’re considering it? This guide is here to walk you through every step, answer your burning questions, and give you a fresh, down-to-earth look at the process—complete with the latest insights and practical tips you won’t find everywhere else.
IVF isn’t just a medical procedure; it’s a journey. Whether you’re dealing with infertility, exploring options as a single parent, or navigating this with a partner, understanding what’s ahead can make all the difference. So, grab a comfy seat, and let’s dive into the world of IVF together.
Why IVF Matters Today
IVF stands for “in vitro fertilization,” which is a fancy way of saying that an egg and sperm are combined outside the body—in a lab dish, to be exact. The resulting embryo is then placed into the uterus to grow into a baby. It’s a lifeline for people who can’t conceive naturally due to blocked fallopian tubes, low sperm count, or other challenges. But it’s also become a go-to for same-sex couples, single folks, and even those who want to freeze their eggs for the future.
What’s wild is how much IVF has evolved. Back in the day, it was experimental and rare. Now, it’s a well-oiled machine, with success rates climbing and new tech making it more accessible. In 2021 alone, nearly 92,000 babies were born via IVF in the U.S., according to the Department of Health and Human Services. That’s about 2.5% of all births! And with people waiting longer to have kids—sometimes into their 30s or 40s—IVF is more relevant than ever.
But here’s the thing: it’s not a one-size-fits-all solution. Every journey is unique, and that’s why knowing the ins and outs can help you feel more in control.
How Does IVF Work? A Step-by-Step Breakdown
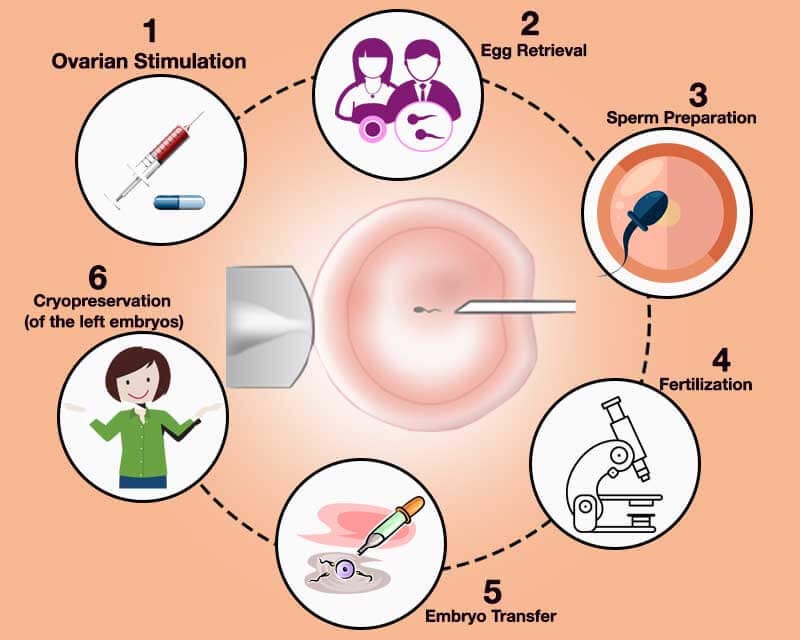
The IVF process is like a carefully choreographed dance with several stages. It usually takes about 4 to 6 weeks for one full cycle, though it can vary. Here’s what happens, broken down into bite-sized steps so it’s easy to follow.
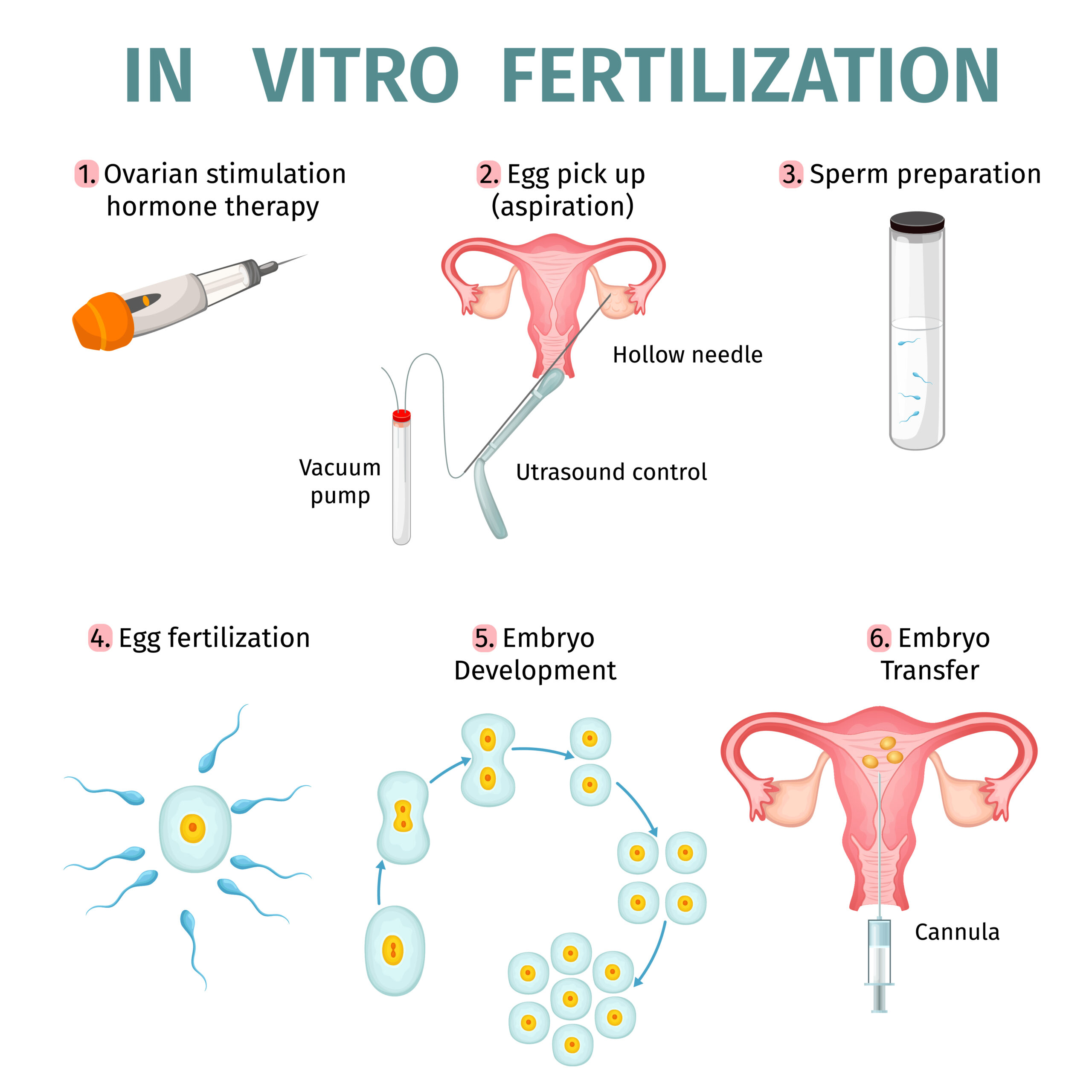
Step 1: Boosting Egg Production
First up, your doctor will prescribe fertility drugs to kick your ovaries into high gear. Normally, your body releases one egg a month, but with IVF, the goal is to produce several at once. More eggs mean more chances for success.
- What to Expect: You’ll take pills or give yourself shots (don’t worry, they’re tiny needles) for about 10-14 days. Your doctor will check in with ultrasounds and blood tests to see how your eggs are growing.
- Fun Fact: These meds mimic hormones your body already makes, like follicle-stimulating hormone (FSH). It’s like giving your ovaries a pep talk!
- Tip: Keep a small cooler handy for storing injectable meds if you’re on the go—they often need to stay cold.
Step 2: Collecting the Eggs
Once your eggs are ready, it’s time for retrieval. This is a quick procedure—about 20 minutes—done under light anesthesia so you’re comfy and snoozing.
- How It Works: A doctor uses a thin needle guided by ultrasound to gently pull the eggs from your ovaries through your vagina. No big cuts or scars here!
- What It Feels Like: You might have some cramping afterward, but most people are back to normal within a day.
- Cool Stat: On average, 10-15 eggs are collected, though it depends on your age and health, per the American Society for Reproductive Medicine.
Step 3: Fertilizing the Eggs
Now, the magic happens in the lab. The eggs meet the sperm—either from your partner or a donor—in a dish. There are two ways this can go:
- Standard IVF: Sperm and eggs are mixed together and left to do their thing overnight.
- ICSI (Intracytoplasmic Sperm Injection): If sperm quality is low, a single sperm is injected right into an egg. This boosts the odds of fertilization.
About 60-70% of eggs fertilize successfully, turning into embryos within a day or two.
Step 4: Growing the Embryos
The fertilized eggs—now embryos—hang out in the lab for 3-6 days. Scientists keep an eye on them, making sure they’re developing well.
- Day 3 vs. Day 5: Some embryos are transferred at the cleavage stage (Day 3), while others grow to the blastocyst stage (Day 5 or 6). Day 5 transfers often have higher success rates because the strongest embryos stand out.
- Pro Tip: Ask your clinic about embryo grading—it’s like a report card that shows which ones are thriving.
Step 5: Transferring the Embryo
Time to put the embryo where it belongs! This step is simple and feels a bit like a Pap smear—no anesthesia needed.
- How It’s Done: A thin tube slides through your cervix to place the embryo in your uterus. You’ll lie back for a bit afterward to let it settle.
- How Many?: Usually 1-2 embryos are transferred, depending on your age and situation. Extra embryos can be frozen for later.
- Success Boost: Some clinics use ultrasound to guide the placement for pinpoint accuracy.
Step 6: The Two-Week Wait
Now, you wait. About 10-14 days later, a blood test checks for pregnancy by measuring hCG (the pregnancy hormone).
- What to Do: Rest, but don’t stress—light activity is fine. Binge a show, read a book, or take walks to keep your mind busy.
- What to Avoid: Heavy lifting or super intense workouts. Your body’s doing important work!
If it’s positive, congrats—you’re on your way! If not, you and your doctor can plan the next steps.
Who Can Benefit from IVF?
IVF isn’t just for one type of person. It’s a versatile tool that helps all kinds of people build families. Here are some common reasons folks turn to it:
- Blocked or Damaged Fallopian Tubes: If the tubes are scarred (say, from an infection), sperm can’t reach the egg naturally.
- Low Sperm Count or Motility: When sperm struggle to swim or there aren’t enough of them, IVF (especially with ICSI) can step in.
- Age-Related Infertility: Fertility drops after 35, and IVF can help by using your eggs, donor eggs, or frozen ones from your younger years.
- Unexplained Infertility: Sometimes, there’s no clear reason you’re not conceiving—IVF can bypass the mystery.
- Single Parents or Same-Sex Couples: With donor sperm, eggs, or surrogates, IVF opens doors for all family types.
Fun fact: In Israel, IVF is so common that they do 1,657 cycles per million people each year—the highest rate in the world! It shows how this process has become a global game-changer.
What’s the Success Rate? Real Numbers, Real Talk
Success is the big question, right? The truth is, it depends on a bunch of factors—your age, health, and even luck. Here’s a breakdown based on 2021 data from the Society for Assisted Reproductive Technology:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 45% |
| 35-37 | 32% |
| 38-40 | 20% |
| 41-42 | 10% |
| Over 42 | 3% |
- Younger Age, Better Odds: Women under 35 have the best shot because egg quality is higher.
- Older Age, Tougher Road: After 40, success drops, but donor eggs can bump it back up to 50% or more.
- Fresh vs. Frozen: Frozen embryo transfers are now just as successful as fresh ones—sometimes even better—thanks to improved freezing tech.
Here’s a quick quiz to keep you engaged:
Mini Quiz: What’s Your IVF IQ?
- What’s the biggest factor in IVF success?
a) The doctor’s skill
b) Your age
c) The clinic’s location - How long does a typical IVF cycle take?
a) 2 weeks
b) 4-6 weeks
c) 3 months
(Answers: 1-b, 2-b. How’d you do?)

The Emotional Side of IVF: What No One Tells You
IVF isn’t just about needles and lab dishes—it’s an emotional rollercoaster. You might feel hopeful one day and crushed the next. That’s normal, and you’re not alone.
The Highs and Lows
- Hope: Every step feels like a win—eggs retrieved, embryos growing, a positive test.
- Heartache: A failed cycle or miscarriage (about 15% of IVF pregnancies end this way) can hit hard.
Coping Tips
- Build a Support Squad: Lean on friends, family, or online communities. There’s strength in sharing.
- Take Breaks: If it’s too much, pause between cycles. Your mental health matters.
- Try Journaling: Writing down your feelings can lighten the load—studies show it reduces stress.
One thing you won’t find in most articles? The guilt factor. Some people feel guilty for “needing” IVF or worry they’re letting their partner down. Spoiler: It’s not your fault. Infertility affects 1 in 8 couples, and IVF is just a tool to help.
Costs and Coverage: Breaking Down the Price Tag
IVF isn’t cheap, and that’s a big hurdle for many. In the U.S., one cycle averages $15,000-$20,000, not counting meds (another $3,000-$5,000). But costs vary wildly by location and clinic.
What’s Included?
- Fertility drugs
- Ultrasounds and blood tests
- Egg retrieval and lab work
- Embryo transfer
Can You Afford It?
- Insurance: Only 19 states mandate some IVF coverage, so check your plan. Even then, it might only cover part of it.
- Grants: Groups like Baby Quest offer financial help—worth a look!
- Mini IVF: A lower-dose, cheaper option ($5,000-$7,000) that’s gaining traction for some patients.
Here’s a fresh angle: In low- and middle-income countries, IVF can cost 50% of a person’s annual income, per a 2023 study in Human Reproduction Open. New efforts, like simplified protocols, are trying to bring prices down globally.