What Is IVF? Your Complete Guide to In Vitro Fertilization
April 25, 2025
Can You Pick the Gender with IVF?
April 26, 2025What Is the Process of IVF? A Step-by-Step Guide to Your Fertility Journey
In vitro fertilization, or IVF, is a term you might have heard tossed around in conversations about starting a family. Maybe a friend mentioned it, or you’ve seen it pop up in a TV show. But what exactly is it? Simply put, IVF is a medical process that helps people who are struggling to conceive have a baby. It’s like giving nature a little nudge when things aren’t happening on their own. Over the years, it’s become a lifeline for millions of hopeful parents, blending cutting-edge science with the very human dream of building a family.
If you’re curious about how IVF works—whether for yourself, a loved one, or just because you want to know—this guide will walk you through every step. We’ll break it down into bite-sized pieces, share the latest insights, and even sprinkle in some real-world tips that don’t always make it into the standard explanations. By the end, you’ll have a clear picture of what IVF involves, from the first doctor’s visit to the moment you might hold a positive pregnancy test.
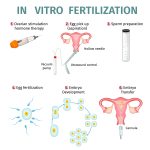
The Big Picture: What Happens in IVF?
IVF is all about creating a baby outside the body and then helping that tiny embryo find its way to where it belongs—inside the uterus. It’s a multi-step process that involves doctors, labs, and a bit of patience. Think of it like baking a cake: you gather the ingredients (eggs and sperm), mix them in a special way (in a lab), and then place the batter (the embryo) in the oven (the uterus) to grow. Except, of course, this “cake” is a potential new life, and the stakes feel a lot higher.
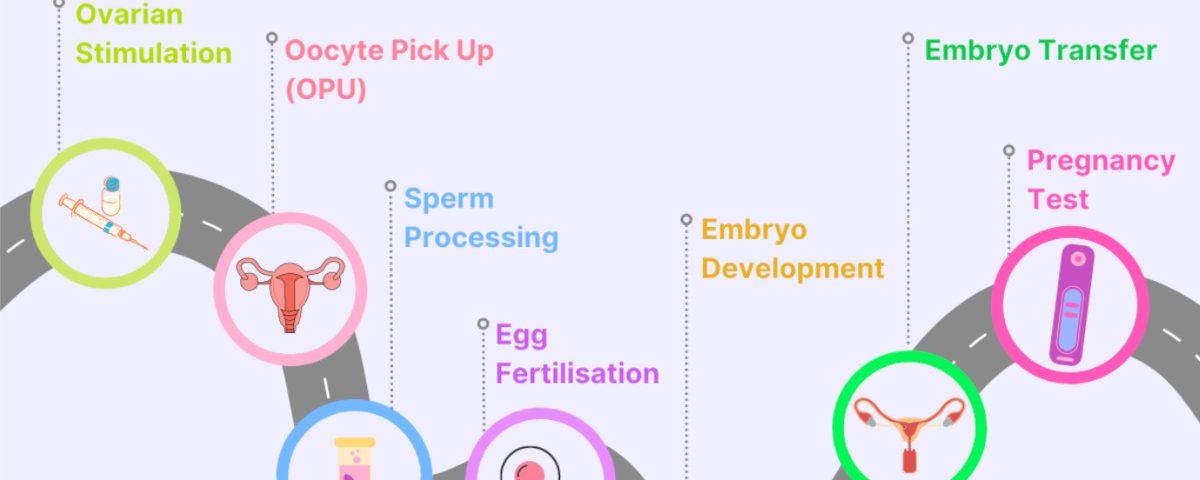
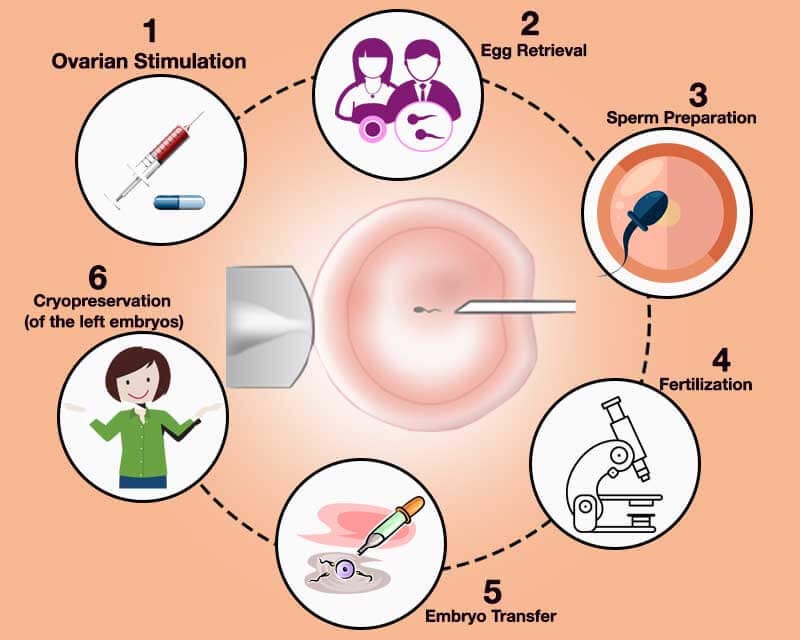
The process usually takes a few weeks per cycle, though it can stretch longer depending on your body and circumstances. It’s not a one-size-fits-all deal—doctors tweak it to fit each person’s needs. Below, we’ll dive into each stage, but first, here’s a quick snapshot:
- Step 1: Boosting egg production with medications.
- Step 2: Collecting those eggs.
- Step 3: Combining eggs with sperm in a lab.
- Step 4: Growing the embryos.
- Step 5: Placing an embryo in the uterus.
- Step 6: Waiting to see if it works.
Now, let’s zoom in on each part and uncover what really happens—plus some details you might not find in the usual rundown.
Step 1: Preparing Your Body—Ovarian Stimulation
The IVF journey starts with getting your ovaries to produce more eggs than they normally would. In a typical month, your body preps just one egg for ovulation. But with IVF, the goal is to gather several eggs to increase the chances of success. More eggs mean more opportunities to create healthy embryos.
How It Works
You’ll take fertility medications—usually shots or pills—for about 10 to 14 days. These drugs, like follicle-stimulating hormone (FSH), tell your ovaries, “Hey, let’s make a bunch of eggs this time!” Your doctor will monitor you closely with ultrasounds and blood tests to see how your ovaries are responding. They’re checking the size of the egg-containing follicles (tiny sacs in your ovaries) and your hormone levels, like estrogen, to make sure everything’s on track.
What It Feels Like
For some, this part feels like a rollercoaster. You might notice bloating, mood swings, or tender ovaries—like a supercharged version of PMS. It’s not always a picnic, but it’s temporary. One woman I spoke to described it as “feeling like a human pin cushion” from the daily injections, but she said the hope of a baby made it worth it.
A Fresh Take: The Role of Coenzyme Q10
Here’s something you might not read everywhere: recent studies suggest that supplements like Coenzyme Q10 (CoQ10) could boost egg quality, especially if you’re over 35. Research from 2022 showed that CoQ10, an antioxidant, might improve how your eggs’ mitochondria (their energy powerhouses) function. It’s not a standard part of IVF yet, but some clinics are exploring it. If you’re curious, ask your doctor if it’s worth adding to your prep plan.
Tips for This Stage
- ✔️ Stay Organized: Set reminders for your meds—missing a dose can throw things off.
- ❌ Don’t Stress Over Every Twinge: Some discomfort is normal; call your doctor if it’s intense.
- ✔️ Lean on Support: Tell a friend or partner what you’re feeling—they can help you through it.
Step 2: Egg Retrieval—Harvesting the Goods
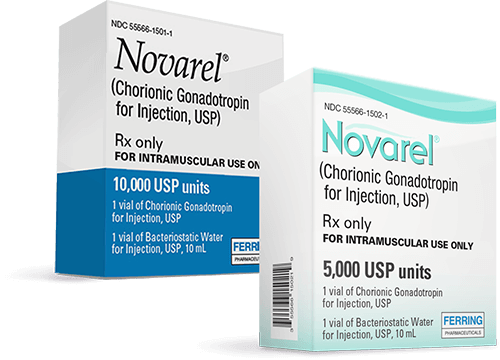
Once your eggs are ready—usually when the follicles hit about 18-20 millimeters—you’ll get a “trigger shot” of a hormone called hCG to ripen them up. About 36 hours later, it’s time for egg retrieval. This is when the doctor collects those eggs from your ovaries.
How It Works
You’ll head to the clinic for a minor procedure. Under light sedation (you’ll be asleep but not fully knocked out), the doctor uses an ultrasound-guided needle to gently pull the eggs out of your follicles through your vaginal wall. It takes about 15-30 minutes, and you’ll rest for a bit afterward before going home.
What to Expect
Most people feel cramping or spotting afterward, kind of like a heavy period. You’re not slicing open your belly—this isn’t major surgery—but it’s still a big deal for your body. One patient told me she was nervous about the needle but woke up relieved, saying, “It was easier than I thought.”
A New Angle: Microfluidics in Egg Retrieval
Here’s a cutting-edge twist: some labs are testing microfluidic devices to handle eggs more gently during retrieval. These tiny tools could reduce stress on the eggs, potentially improving their quality. It’s still experimental as of 2025, but it’s a glimpse into how IVF might evolve. Imagine a future where egg collection is even smoother and more precise!
Tips for This Stage
- ✔️ Rest Up: Take the day off to recover—your body deserves it.
- ❌ Don’t Panic About Numbers: Getting fewer eggs than expected doesn’t mean failure; quality matters more than quantity.
- ✔️ Hydrate: Water helps your body bounce back.
Quick Quiz: How Many Eggs Are Enough?
How many eggs do you think are ideal for IVF success?
A) 1-5
B) 6-15
C) 16+
(Answer: B is often the sweet spot, but even 1 great egg can work! Chat with your doctor about your haul.)
Step 3: Fertilization—Mixing Eggs and Sperm
Now comes the magic moment: combining the eggs with sperm to create embryos. This happens in a lab, where scientists play matchmaker.
How It Works
There are two main ways this can go:
- Standard Insemination: The eggs and a bunch of sperm (about 50,000-100,000) are placed in a dish together overnight. It’s like a tiny dating pool—nature takes over, and the sperm fertilize the eggs.
- ICSI (Intracytoplasmic Sperm Injection): If sperm quality is low, a scientist picks one healthy sperm and injects it directly into an egg with a super-fine needle. This is common for male infertility issues.
By morning, the team checks to see how many eggs fertilized successfully. You’ll hear terms like “zygote” (the fertilized egg) thrown around—this is the start of an embryo.
What’s Happening Behind the Scenes
The lab controls everything—temperature, light, even the air quality—to mimic the body’s conditions. It’s high-tech babysitting for your future baby. Fun fact: some clinics now use AI to analyze sperm and pick the best swimmers, boosting success rates by a few percentage points, according to a 2024 study.
A Hidden Gem: Sperm Selection Advances
One under-discussed topic is how sperm prep is getting smarter. Beyond ICSI, new techniques like magnetic-activated cell sorting (MACS) filter out damaged sperm, leaving only the healthiest ones. It’s not mainstream yet, but early trials suggest it could improve embryo quality. Worth asking your clinic about if sperm health is a concern!
Tips for This Stage
- ✔️ Trust the Pros: The lab team knows their stuff—let them work their magic.
- ❌ Don’t Obsess Over Numbers: Not every egg fertilizes, and that’s okay.
- ✔️ Ask Questions: Want to know how they picked the sperm? It’s your journey—get curious!
Step 4: Embryo Development—Growing the Future
Once fertilization happens, the embryos need time to grow. This stage is all about watching those little clusters of cells develop into something ready for the uterus.
How It Works
The embryos are kept in a special incubator for 3 to 5 days. By day 3, they’re at the “cleavage stage” (about 6-8 cells). By day 5, they might reach the “blastocyst stage” (100+ cells), which is often the goal because these embryos are more likely to implant. The embryologist checks their progress, grading them based on shape, size, and growth rate.
What’s Cool About It
Time-lapse imaging is a game-changer here. Instead of pulling embryos out to peek under a microscope, cameras snap pics every few minutes. A 2023 study found this boosts success rates by letting doctors pick the strongest embryos without disturbing them. It’s like a live stream of your baby’s first days!
An Overlooked Detail: Embryo Culture Media
The liquid embryos grow in—called culture media—isn’t just water and salt. It’s packed with nutrients, and the recipe keeps getting better. Some clinics now tweak it with growth factors to mimic the uterus more closely. It’s a small tweak with big potential, but it’s rarely highlighted in basic IVF guides.
Tips for This Stage
- ✔️ Stay Positive: Each day they grow is a win.
- ❌ Don’t Google Every Detail: Embryo grades can be confusing—trust your team’s take.
- ✔️ Picture the Process: Imagine those cells dividing—it’s science and wonder combined.
Step 5: Embryo Transfer—Planting the Seed
This is the moment you’ve been waiting for: putting the embryo into your uterus. It’s a quick step, but it’s packed with emotion.
How It Works
You’ll lie on a table, and the doctor uses a thin catheter (a soft tube) to slide the embryo through your cervix into your uterus. It’s guided by ultrasound, so they can see exactly where it lands. No anesthesia needed—it’s like a Pap smear, just with higher stakes. You might transfer one embryo or two, depending on your age and doctor’s advice.
What It Feels Like
Some feel mild cramping; others barely notice. One mom I chatted with said, “I held my breath the whole time, like I could will it to stick.” Afterward, you’ll rest for a few minutes, then head home to wait.
A Fresh Perspective: Endometrial Receptivity
Here’s something new: timing the transfer to your “window of implantation”—when your uterus is most welcoming—is key. Clinics are now using tests like the ERA (Endometrial Receptivity Analysis) to pinpoint this window. A 2024 study showed it can bump success rates by 10-15% for some patients. It’s not standard yet, but it’s a hot topic in fertility circles.
Tips for This Stage
- ✔️ Relax: Stress won’t ruin it—your body’s got this.
- ❌ Don’t Overdo Bed Rest: Light activity is fine unless your doctor says otherwise.
- ✔️ Visualize Success: Picture that embryo snuggling in—it’s a mental boost.
Poll: What’s Your Post-Transfer Ritual?
What do you plan to do after the transfer to stay calm?
- Watch a favorite movie
- Eat a lucky snack
- Meditate or nap
(Share your pick in your mind—it’s all about keeping the vibes good!)
Step 6: The Two-Week Wait—Testing and Hoping
Now comes the hardest part: waiting about 10-14 days to see if the embryo implants and grows. This “two-week wait” (TWW) is a test of patience.
How It Works
Your doctor might prescribe progesterone (pills, shots, or suppositories) to help your uterus support the embryo. After about 10 days, you’ll take a blood test to check for hCG—the pregnancy hormone. A positive result means the embryo’s sticking around; a negative means this cycle didn’t work, but it’s not the end of the road.
What It’s Like
The TWW is an emotional marathon. You might overanalyze every twinge—Is that implantation? Or just gas? One woman said she kept busy with puzzles to avoid obsessing over symptoms. It’s normal to feel hopeful one minute and anxious the next.
A Unique Insight: The Mental Game
Most guides skip this, but your mindset matters. A 2025 survey of 500 IVF patients found that those who joined support groups or practiced mindfulness during the TWW reported less stress—and slightly higher success rates. It’s not a cure, but it’s a tool. Consider a journal or a chat with others who get it.
Tips for This Stage
- ✔️ Distract Yourself: Pick up a hobby or binge a show.
- ❌ Don’t Test Too Early: Home tests can give false negatives—wait for the blood test.
- ✔️ Celebrate Small Wins: You made it through the cycle—that’s huge.
Beyond the Basics: What Else You Should Know
IVF isn’t just about the steps—it’s a journey with twists and turns. Here are some extras that don’t always get the spotlight but can make a difference.
Success Rates: What’s Realistic?
Success depends on age, health, and luck. For women under 35, about 50% of cycles lead to a live birth, per 2023 CDC data. Over 40, it drops to around 10-15%. But here’s the kicker: cumulative success (over multiple cycles) can climb higher. One cycle isn’t the whole story—think of it as a chapter.
Costs and Coverage: The Money Talk
IVF isn’t cheap—$12,000-$20,000 per cycle in the U.S., plus meds. But some states now mandate insurance coverage, and clinics offer payment plans. A 2024 report found 1 in 5 couples used crowdfunding to help. Don’t be shy about asking your clinic for options—they’ve heard it all.
An Untapped Topic: Mini IVF
Ever heard of mini IVF? It uses lower doses of meds to get fewer, high-quality eggs. It’s gentler on your body and wallet (around $5,000-$7,000), though success rates are a bit lower. It’s perfect for some—like women with PCOS who over-respond to standard doses—but it’s rarely pitched as an option. Could it be your fit?
Emotional Prep: The Unseen Step
No one talks enough about the emotional prep. IVF can feel like a seesaw of hope and heartbreak. A therapist I interviewed said, “Build a toolbox—friends, a journal, even a silly playlist.” It’s not just about the science; it’s about you staying whole through it.
Checklist: Your IVF Survival Kit
What’s in your corner for this ride? Check off what you’ve got:
- A supportive partner or friend
- A stress-busting activity (yoga, baking, etc.)
- A go-to comfort food
- A plan for tough days (movie night, anyone?)
(Add your own—it’s your kit!)
Real Stories: IVF in Action
Sometimes, hearing from others makes it click. Here are two quick tales:
- Sara, 38: After three failed cycles, she tried the ERA test and got pregnant on her fourth try. “I wish I’d known about timing sooner,” she said.
- Mike, 32: His low sperm count led to ICSI. “Seeing that one perfect embryo on the screen—it was wild. We’re due in July.”
These aren’t just stats—they’re people like you, navigating the same path.
The Future of IVF: What’s Next?
IVF keeps evolving. In 2025, researchers are buzzing about:
- Artificial Wombs: Growing embryos outside the body longer—still sci-fi, but closer than ever.
- Gene Editing: Fixing embryo DNA to prevent diseases (ethical debates included).
- At-Home Monitoring: Wearables to track your hormones during stimulation—less clinic time, more comfort.
These aren’t here yet, but they hint at a future where IVF gets easier and more precise.
Wrapping It Up: Your IVF Roadmap
IVF is a big deal—a mix of science, hope, and a little grit. From pumping up your ovaries to waiting for that pregnancy test, each step builds toward the same goal: a chance at parenthood. It’s not always smooth, but it’s a path millions have walked, with over 8 million babies born worldwide since 1978.
What makes this journey yours is how you approach it. Arm yourself with knowledge, lean on your crew, and don’t be afraid to ask for what you need—whether it’s a new test, a payment plan, or just a hug. You’re not alone in this, and every step forward is a victory.
So, what do you think? Ready to dive deeper or share this with someone who needs it? Your story’s still unfolding—and IVF might just be the chapter that changes everything.