Why Is IVF Morally Wrong?
April 26, 2025
Why Does IVF Fail with Good Embryos?
April 26, 2025Can You Have an Ectopic Pregnancy with IVF?
When you’re going through in vitro fertilization (IVF), the hope is to finally hold a healthy baby after months—or even years—of effort. It’s a journey filled with excitement, nerves, and a lot of questions. One question that might pop up, especially if you’ve heard whispers about it, is whether an ectopic pregnancy can happen with IVF. The short answer? Yes, it can. But there’s so much more to unpack here—why it happens, how common it is, what you can do about it, and what the latest research says. Let’s dive in and explore this topic together, step by step, so you feel informed and ready for whatever comes your way.
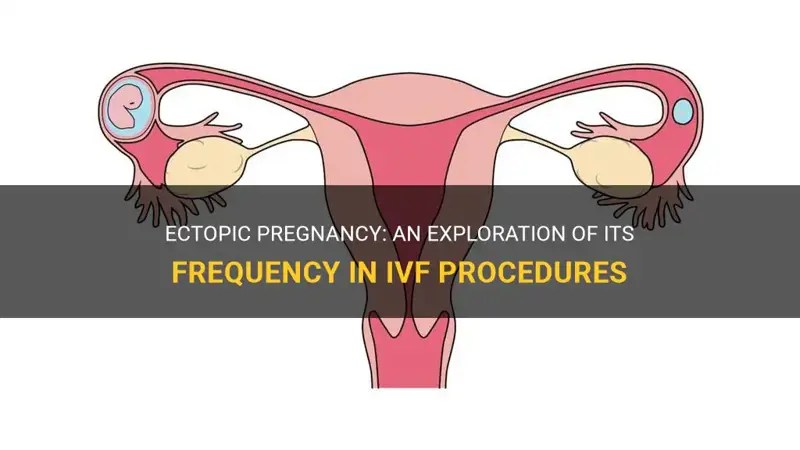
What Is an Ectopic Pregnancy, Anyway?
An ectopic pregnancy happens when a fertilized egg implants somewhere outside the uterus, most often in one of the fallopian tubes. Normally, after conception (whether natural or through IVF), the embryo travels down the tube and settles into the uterus, where it can grow into a baby. But in an ectopic pregnancy, that journey goes off track. The embryo gets stuck or implants in the wrong spot, and since those areas aren’t built to support a growing pregnancy, it can lead to serious complications if not caught early.
With IVF, you might think this wouldn’t happen. After all, doctors place the embryo directly into the uterus, right? So how could it end up somewhere else? That’s a great question—and one we’ll answer as we go along. For now, know that ectopic pregnancies are rare but real, even with IVF, and understanding them can help you feel more in control.
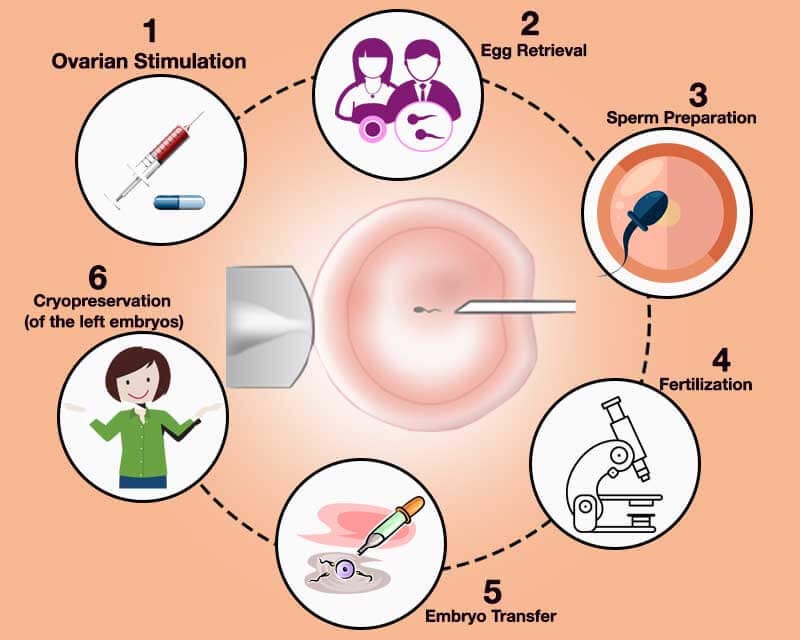
How IVF Works: A Quick Recap
To get why ectopic pregnancies can still happen with IVF, let’s take a quick look at how IVF works. During IVF, doctors stimulate your ovaries to produce multiple eggs, retrieve those eggs, and fertilize them with sperm in a lab. Once the embryos develop, one or more are carefully transferred into your uterus using a thin catheter. The goal is for the embryo to implant in the uterine lining and grow into a healthy pregnancy.
It’s a precise process, guided by ultrasound and years of medical expertise. But even with all that precision, the human body isn’t a perfect machine. Sometimes, things don’t go exactly as planned—and that’s where the risk of an ectopic pregnancy comes in.
Yes, Ectopic Pregnancies Can Happen with IVF—Here’s Why
So, can you have an ectopic pregnancy with IVF? Absolutely. Studies show that ectopic pregnancies occur in about 1.4% to 5.4% of IVF pregnancies, which is higher than the 1% to 2% rate in natural conceptions. That might sound surprising since the embryo is placed right where it needs to be. But there are a few reasons this can still happen:
- Tubal Issues: Many people turn to IVF because of fertility challenges, like damaged or blocked fallopian tubes. Even though the embryo is placed in the uterus, those tubes can still play a role. If they’re scarred or inflamed, the embryo might migrate out of the uterus and into a tube.
- Embryo Movement: Embryos are tiny and mobile. After transfer, they can sometimes drift out of the uterus due to uterine contractions or fluid movement, landing in a fallopian tube or even rarer spots like the ovary or abdomen.
- Transfer Technique: The way the embryo is placed matters. If it’s too close to the top of the uterus (near the tube openings) or if too much fluid is used, it might increase the chance of the embryo wandering off.
- Multiple Embryos: Transferring more than one embryo, which used to be more common, can up the odds of at least one implanting in the wrong place.
These factors don’t mean ectopic pregnancies are inevitable with IVF—they’re still uncommon—but they do explain why the risk isn’t zero.
How Common Are Ectopic Pregnancies with IVF?
Let’s put some numbers on this. Research from the past decade shows that ectopic pregnancies after IVF happen in about 2% to 3% of cases on average. That’s a small percentage, but it’s enough to make you wonder why it’s higher than natural pregnancies. Part of it ties back to the fertility issues that lead people to IVF in the first place—like tubal damage from past infections or surgeries.
Here’s a breakdown based on recent studies:
- Fresh vs. Frozen Transfers: Frozen embryo transfers (FET) tend to have a lower ectopic rate (around 1.5%) compared to fresh transfers (closer to 2.5%). Why? Frozen cycles give the body a break from hormone stimulation, which might make the uterus a more stable landing spot.
- Blastocyst vs. Cleavage Stage: Transferring embryos at the blastocyst stage (day 5) might slightly reduce the risk compared to earlier stages (day 3), though the data isn’t unanimous on this.
- Single vs. Multiple Embryos: Single embryo transfers, now more common, cut the risk compared to transferring two or more.
The good news? These rates have been dropping over time as IVF techniques improve. Still, it’s worth knowing what to watch for.
Quick Quiz: Are You at Risk?
Take a moment to think about your situation. Answer these yes-or-no questions to get a sense of your risk level (don’t worry, this isn’t medical advice—just a starting point!):
- ✔️ Have you had a previous ectopic pregnancy?
- ✔️ Do you have a history of pelvic infections or tubal surgery?
- ✔️ Are you over 35?
- ✔️ Are you doing a fresh embryo transfer with multiple embryos?
If you checked “yes” to any of these, your risk might be a bit higher. Chat with your doctor to dig deeper.
Signs to Watch For: Could It Be Ectopic?
Ectopic pregnancies can be sneaky, especially early on. After IVF, you’re already hyper-aware of every twinge and symptom, so it’s helpful to know what’s normal and what’s not. Here are some red flags to keep an eye on:
- Pain: Sharp or persistent pain on one side of your lower abdomen or pelvis isn’t typical implantation cramping. It might feel different from the usual IVF bloating or soreness.
- Bleeding: Light spotting can happen with implantation, but heavier bleeding—especially with clots—could signal trouble.
- Shoulder Pain: This odd one comes from internal bleeding irritating your diaphragm. It’s rare but serious.
- Dizziness or Fainting: Feeling lightheaded or weak could mean internal bleeding is affecting your blood pressure.
If you notice these, don’t wait—call your doctor right away. Early detection is key to managing an ectopic pregnancy safely.
What to Do If You’re Worried
Caught something that doesn’t feel right? Here’s a simple action plan:
- Track It: Jot down when the symptom started, how it feels, and how long it lasts.
- Call Your Clinic: They’ll likely want to see you for an ultrasound or blood test to check your hCG levels.
- Rest Up: Avoid heavy lifting or strenuous activity until you get answers.
Your peace of mind matters, so don’t hesitate to reach out.
Why Early Detection Matters—and How It’s Done
Catching an ectopic pregnancy early can make all the difference. With IVF, you’re already under close watch, which is a big advantage. Doctors typically monitor you with:
- Ultrasound: Around 5-6 weeks after transfer, they’ll check where the embryo is. A sac outside the uterus is a clear sign.
- hCG Levels: These hormone levels rise slower in ectopic pregnancies than in healthy ones. If they’re not doubling every 48 hours or so, it’s a clue to investigate further.
Fun fact: A 2024 study found that combining ultrasound with hCG trends catches 95% of ectopic pregnancies before they rupture. That’s reassuring! Your IVF team is trained to spot these patterns, so trust their process.
Unique Risks: Beyond the Fallopian Tubes
Most ectopic pregnancies land in the tubes, but IVF can lead to some rare twists. These don’t get as much attention, so let’s shine a light on them:
- Abdominal Ectopic: The embryo implants in the belly cavity. It’s super rare (less than 1% of ectopics), but it’s been linked to IVF cases where tubes were removed or damaged.
- Cervical Ectopic: The embryo settles in the cervix. This can happen if the transfer catheter goes too low.
- Heterotopic Pregnancy: This is a wild one—an ectopic pregnancy and a uterine pregnancy at the same time. It’s more likely with IVF (about 1 in 100 cases) because of multiple embryo transfers.
These oddballs are why your doctor might double-check everything, even if you feel fine.
Real Story: Sarah’s Surprise
Sarah, a 32-year-old IVF patient, felt thrilled when her pregnancy test was positive. But at her 6-week ultrasound, the doctor found a healthy uterine pregnancy and a small mass in her tube—a heterotopic pregnancy. Quick surgery removed the ectopic while saving her uterine baby. She’s now mom to a healthy girl and shares her story to remind others: weird things can happen, but modern medicine can handle it.
What Increases Your Risk with IVF?
Not everyone has the same odds of an ectopic pregnancy with IVF. Some factors bump up the risk:
- Past Ectopic: If you’ve had one before, your risk jumps to 6-8% with IVF.
- Tubal Damage: Scarring from infections, endometriosis, or surgery makes it harder for embryos to stay put.
- Age: Over 35? The risk creeps up slightly, possibly due to changes in tube function.
- Smoking: It messes with tube movement, increasing ectopic odds by 2-3 times.
- Fresh Transfers: The hormone overload might make the uterus less “sticky” for embryos.
On the flip side, newer IVF trends—like single embryo transfers and frozen cycles—seem to lower the risk. It’s all about finding what works for you.
Risk Comparison Table
| Factor | Ectopic Risk Increase | Why It Happens |
|---|---|---|
| Past Ectopic | 3-4x higher | Tubes may still be compromised |
| Tubal Damage | 2-3x higher | Scarring traps embryos |
| Fresh Transfer | 1.5x higher | Hormones affect implantation |
| Multiple Embryos | 2x higher | More chances for misplacement |
Can You Prevent an Ectopic Pregnancy with IVF?
Prevention isn’t foolproof, but there are steps to lower your risk:
- Opt for Frozen Transfers: Studies show a 30-50% drop in ectopic rates with FET. Your body gets time to reset.
- Stick to One Embryo: Single transfers reduce the chance of an embryo going rogue.
- Fix Tubal Issues: If you’ve got damaged tubes, talk to your doctor about removing them (salpingectomy) before IVF. It’s not for everyone, but it can cut risk.
- Quit Smoking: Easier said than done, but it’s a game-changer for tube health.
Your clinic might tweak their approach—like adjusting catheter placement—to help, too.
Myth vs. Fact
- ❌ Myth: IVF eliminates ectopic risk because the embryo goes straight to the uterus.
Fact: Embryos can still move after transfer. - ✔️ Fact: Frozen transfers lower the risk compared to fresh ones.
Data backs this up—ask your doctor about it!
Treatment Options: What Happens If It’s Ectopic?
If an ectopic pregnancy is confirmed, the focus shifts to keeping you safe. Here’s how it’s handled:
- Medication (Methotrexate): For early, stable cases, this drug stops the pregnancy from growing. You’ll need follow-ups to ensure it works.
- Surgery: If it’s ruptured or too big, laparoscopy removes the ectopic tissue. Tubes can often be saved, preserving future fertility.
- Watchful Waiting: Super rare, but if it’s tiny and hCG is dropping, your body might resolve it naturally.
Your doctor will tailor the plan to your situation—your health comes first.
Recovery Checklist
After treatment, here’s what to do:
- ✔️ Rest for a few days (or weeks if it’s surgery).
- ✔️ Follow up with hCG tests to confirm it’s gone.
- ❌ Avoid pregnancy for 3 months if you used methotrexate.
- ✔️ Talk to your doctor about your next IVF try.
Emotional Impact: Coping with the Unexpected
An ectopic pregnancy can hit hard emotionally, especially after the rollercoaster of IVF. You might feel disappointed, scared, or even guilty (though it’s not your fault). It’s okay to grieve that loss. Here’s how to navigate it:
- Lean on Support: Talk to your partner, a friend, or a counselor who gets it.
- Join a Group: Online forums or IVF support groups can connect you with others who’ve been there.
- Give Yourself Time: Healing isn’t linear—take it day by day.
One woman I heard about kept a journal after her ectopic. She said writing down her fears helped her let them go and focus on her next step.
What’s New in 2025: Latest Research Insights
Research is always evolving, and 2025 has brought some fresh takes on ectopic pregnancies with IVF:
- Endometrial Thickness Matters: A study this year found that a thinner lining (under 8 mm) during transfer ups the ectopic risk by 15%. Thicker linings seem to anchor embryos better.
- AI Prediction Tools: Some clinics are testing algorithms to predict ectopic risk based on your history and transfer details. Early results are promising—80% accuracy!
- Tube Removal Debate: New data suggests removing damaged tubes before IVF cuts ectopic rates by 40%, but it’s a big decision. More studies are underway.
These findings could shape how your doctor plans your cycle, so ask about what’s cutting-edge at your clinic.
Poll: What’s Your Take?
What do you think about removing tubes to lower ectopic risk?
- A) Worth it for peace of mind.
- B) Too drastic—I’d rather not.
- C) I’d need more info first.
Drop your vote in your head (or share with a friend) and see where you land!
A Deeper Dive: Why IVF Ectopics Are Different
Ectopic pregnancies with IVF aren’t quite like natural ones. For one, the embryo’s starting point is controlled, yet it can still veer off. Researchers think the lab environment might play a role—embryos grown in vitro could have subtle differences in how they implant. Plus, the hormone cocktails used in IVF might tweak uterine conditions, making it less “sticky” in some cases.
Another angle? The stress of infertility itself. Chronic stress can affect tube function, though this link is still being explored. It’s a reminder that IVF is a marvel of science, but it’s working with the unpredictable beauty of biology.
Your Next Steps: Talking to Your Doctor
Armed with all this info, you’re ready to have a solid chat with your IVF team. Here are some questions to bring up:
- “Based on my history, am I at higher risk for an ectopic?”
- “Should we go with a frozen transfer to lower the odds?”
- “What’s your plan if we spot something off early?”
Write down their answers—it’ll help you feel on top of things.
Actionable Tips for Your IVF Journey
- ✔️ Ask for an ultrasound 5-6 weeks post-transfer, even if you feel great.
- ✔️ Track your symptoms daily in a notebook or app.
- ❌ Don’t ignore weird pain—better safe than sorry.
The Big Picture: Hope Beyond the Risk
Here’s the bottom line: Yes, ectopic pregnancies can happen with IVF, but they’re a small piece of the puzzle. Most IVF pregnancies—over 97%—implant right where they should. Advances in technology, like better transfer techniques and personalized protocols, are shrinking the risk every year. You’re not alone in this—your doctors, nurses, and support network are there to guide you.
Think of it like planting a garden. Sometimes a seed blows off course, but with care and attention, most take root and bloom. Your IVF journey might have bumps, but the chance to grow your family is worth every step.
So, take a deep breath, ask your questions, and keep moving forward. You’ve got this—and science has your back.