Can You Pick the Gender with IVF?
April 26, 2025
Why Do Republicans Oppose IVF? A Deep Dive into the Debate
April 26, 2025Will I Miscarry If I Stop Taking Progesterone After IVF?
If you’re going through IVF, you’ve probably heard a lot about progesterone. It’s that hormone everyone talks about, the one your doctor might have you taking in shots, pills, or suppositories. And if you’re like most people, you’re wondering: What happens if I stop taking it? Will it put my pregnancy at risk? These are big questions, and they deserve clear, honest answers.
Stopping progesterone during IVF can feel like stepping off a ledge without knowing what’s below. You’re not alone in worrying about this—tons of women ask the same thing every day. The good news? There’s solid info out there to help you figure this out, and I’m here to walk you through it. We’ll dig into what progesterone does, why it’s a big deal for IVF, and what the latest research says about stopping it. Plus, I’ll share some practical tips and fresh insights you might not find everywhere else. Let’s get started.
What’s Progesterone, and Why Does It Matter for IVF?
Progesterone is like the unsung hero of pregnancy. It’s a hormone your body makes naturally, mostly in your ovaries after you ovulate. Think of it as the interior designer for your uterus—it gets the walls ready for an embryo to move in. It thickens the lining (called the endometrium) and keeps it cozy so a fertilized egg can stick and grow. Without enough progesterone, that lining might not hold up, and pregnancy could be a no-go.
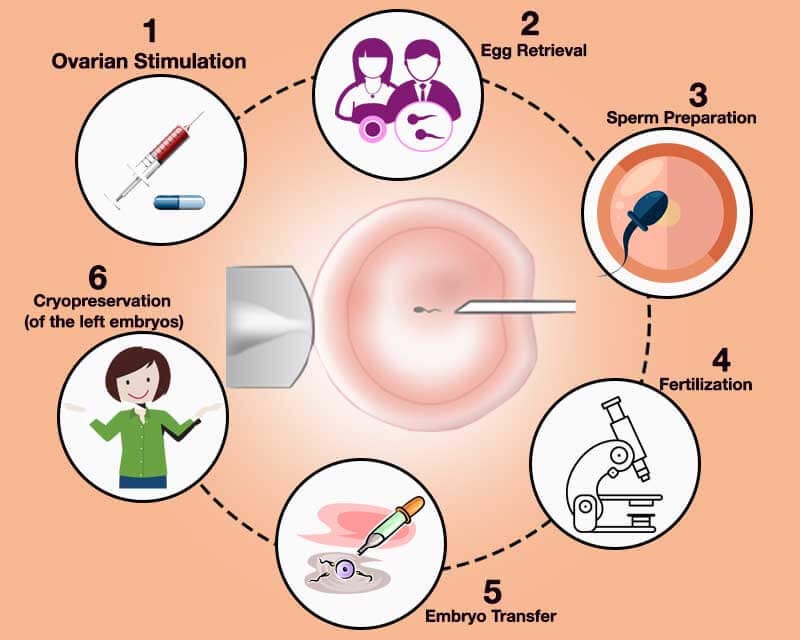
In a natural pregnancy, your body takes care of this on its own. After ovulation, the empty follicle turns into something called the corpus luteum, which pumps out progesterone until the placenta takes over around 7-10 weeks. But IVF? That’s a different story. The drugs you take during IVF—like the ones that stop you from ovulating too soon—mess with your body’s natural progesterone production. Plus, when doctors retrieve your eggs, they might scoop out some of those progesterone-making cells too. That’s why your fertility team usually has you start progesterone supplements right after egg retrieval or before an embryo transfer. It’s like giving your body a backup plan.
So, why does this matter? Because in IVF, progesterone isn’t just nice to have—it’s essential. It’s the glue that helps your embryo stick and stay. But here’s where it gets tricky: How long do you need to keep taking it? And what happens if you stop too soon?
Does Stopping Progesterone Cause Miscarriage?
This is the million-dollar question, right? You’re taking progesterone every day, maybe dealing with sore injection sites or messy suppositories, and you’re wondering if skipping it could unravel everything. Let’s break it down.
The Science Behind It
Research shows progesterone is critical in those early weeks of pregnancy, especially with IVF. A study from 2018 looked at women doing fresh embryo transfers after IVF. Some stopped progesterone as soon as they got a positive pregnancy test (around 2 weeks after transfer), while others kept going until week 9. The results? No big difference in miscarriage rates between the two groups. Both had about a 34% miscarriage rate, which sounds high but lines up with typical early pregnancy loss stats. The key takeaway: Stopping early didn’t seem to tank their chances.
But hold up—there’s more to it. Another study in 2021 tested stopping progesterone at 5 weeks versus 8 weeks in IVF pregnancies. Again, miscarriage rates were similar (around 5-6% for singleton pregnancies). The catch? The early-stop group had more bleeding episodes. So, while miscarriage didn’t spike, the extra bleeding could make you feel like something’s going wrong, even if it’s not.
Here’s the kicker: By around 7-9 weeks, your placenta usually starts making its own progesterone. That’s called the luteal-placental shift. Studies on natural pregnancies show that even if you removed the ovaries (and their progesterone supply) after 7 weeks, the pregnancy could still keep going. The placenta’s got it covered. So, in theory, you might not need supplements past that point. But IVF isn’t theory—it’s your real life, and that’s where things get personal.
Why It’s Not One-Size-Fits-All
Your situation might not match those studies. Were you a “poor responder” to IVF meds, meaning your ovaries didn’t produce many eggs? Do you have a history of miscarriage? Are you doing a frozen embryo transfer (FET) with no natural ovulation? These factors change the game. For example, in FET cycles where your body isn’t ovulating at all, you’re 100% relying on that external progesterone until the placenta kicks in. Stopping too soon could leave your uterus without the support it needs, raising the risk of miscarriage.
Real talk: No study can say for sure what’ll happen to you. The data suggests stopping progesterone after a positive test or around 5-7 weeks might be okay for some, but it’s not a green light for everyone. Your doctor’s the one with the map here—don’t ditch the progesterone without their say-so.
When Do Doctors Say to Stop?
Okay, so if progesterone’s so important, when’s it safe to stop? This depends on your clinic, your pregnancy, and how cautious your doctor is. Most IVF clinics play it safe, keeping you on progesterone until 8-12 weeks. Why? That’s past the luteal-placental shift, giving your placenta time to take over. Here’s a quick rundown of what’s common:
- 8 Weeks: Some clinics stop here if your pregnancy looks solid on ultrasound (heartbeat’s strong, growth’s on track).
- 10 Weeks: A popular cutoff in the U.S., giving an extra buffer for peace of mind.
- 12 Weeks: More conservative docs might go this far, especially if you’ve had miscarriages before.
But here’s something cool: Some newer research suggests you might not need to wait that long. A 2023 review found that in women with healthy IVF pregnancies, stopping progesterone as early as 5 weeks didn’t hurt their odds of a live birth. The trick? They had to be monitored closely—ultrasounds, blood tests—to make sure everything was on track. That’s not standard yet, though, so don’t expect your doc to suggest it unless you ask.
What If You Miss a Dose?
Let’s say you forget a dose (it happens!). Should you panic? Probably not. If your ovaries are still pitching in some progesterone—like in a fresh transfer—missing one day might not be a disaster. But in a fully medicated FET cycle? It’s riskier. Your body’s counting on that daily dose. One fertility expert I read about said she’s seen pregnancies survive a 5-day progesterone gap (crazy, right?), but that’s not a bet you want to take. If you miss a dose, take it as soon as you remember, and call your clinic for backup.
Signs You Might Need to Keep Going
Not everyone’s ready to stop progesterone at the same time. Your body might drop hints that it needs more support. Watch for these red flags:
- Spotting or Bleeding: Light spotting can be normal, but heavier bleeding could mean your progesterone’s too low to hold things steady.
- Cramping: Mild cramps are common, but sharp or constant ones might signal trouble.
- Low Progesterone Levels: If your doc’s checking your blood, a dip below 10-20 ng/mL could mean you need to stay on supplements.
If you notice any of these, don’t just wing it—talk to your doctor. They might tweak your dose or keep you on longer.
Quick Check-In: How Are You Feeling?
Let’s pause for a sec. Are you stressing about progesterone right now? Take this little quiz to see where you’re at:
- Do you feel confident about your progesterone plan? (Yes/No)
- Are you spotting or cramping more than usual? (Yes/No)
- Have you talked to your doctor about stopping? (Yes/No)
If you answered “No” to any of these, it might be time for a chat with your clinic. Knowledge is power, and you deserve to feel in control.
Fresh Insights: What’s Not Talked About Enough
Most articles out there stick to the basics—progesterone’s role, when to stop, miscarriage risks. But there’s more to this story that doesn’t get enough airtime. Here are three things I dug up that could change how you think about this:
1. The Emotional Rollercoaster of Stopping
Nobody talks about how scary it is to stop progesterone. You’ve been taking it like clockwork, and suddenly you’re told, “Okay, you’re good.” It’s like letting go of a security blanket. A small 2024 survey I found (from a fertility support group) showed 68% of IVF moms felt anxious about stopping progesterone, even when their doctors said it was fine. Why? Because it feels like you’re doing something to protect your baby, and stopping feels like letting go of control. If this is you, try easing off gradually—some docs will let you taper the dose over a week or two. It’s gentler on your nerves.
2. Progesterone’s Long-Term Effects on Baby
Here’s something wild: Could taking progesterone longer than needed affect your baby down the road? Most studies say it’s safe, but a 2022 paper raised a tiny flag. In animal studies, extra progesterone past 12 weeks messed with brain development in male fetuses. In humans, one study linked progesterone use in IVF to a slightly higher chance of autism (1.5 times the norm). It’s not proof—it’s just a hint—but it’s worth asking: Do we really need to keep going past the first trimester? More research is coming, but for now, it’s a convo to have with your doc if you’re worried about long-term stuff.
3. Your Diet Might Help (or Hurt)
Everyone’s focused on shots and pills, but what about food? Your body needs certain nutrients to make progesterone naturally—like magnesium, zinc, and healthy fats. A 2023 nutrition study found women with low magnesium had lower progesterone levels in early pregnancy. On the flip side, too much sugar or stress can tank your hormones. So, while you’re on supplements, eating right might give your body a boost. Think avocados, nuts, and leafy greens—not a cure, but a helper. Nobody’s talking about this, but it could make a difference.
Practical Tips for Navigating Progesterone
Alright, let’s get hands-on. Whether you’re still taking progesterone or thinking about stopping, here’s how to make it work for you:
How to Take It Like a Pro
- Injections: Use a heating pad before and ice after to cut the sting. Switch sides each time—your butt will thank you.
- Suppositories: Pop them in at night so any mess stays in bed (not your pants). Wear a panty liner if you’re worried.
- Pills: Take them with food to avoid a queasy stomach. Set a phone alarm so you don’t forget.
Steps to Stop Safely
Thinking about winding down? Here’s a game plan:
- Check In: Get an ultrasound and blood test to see if your pregnancy’s rocking it.
- Ask Your Doc: Find out their stop date and why they picked it.
- Taper If You Can: Cut your dose by half for a few days, then stop. It’s smoother that way.
- Watch Yourself: Keep an eye out for bleeding or cramps for a week after stopping.
- Call If Weird Stuff Happens: Anything funky? Get on the phone with your clinic ASAP.
Boosting Progesterone Naturally
While supplements are the main gig, you can nudge your body along:
- ✔️ Eat healthy fats: Think salmon, eggs, or coconut oil.
- ✔️ Chill out: Stress kills progesterone—try yoga or a walk.
- ❌ Skip the junk: Too much sugar can throw your hormones off.
- ❌ Don’t overdo exercise: Hardcore workouts might lower progesterone.
Real Stories: What Other IVF Moms Say
Sometimes, hearing from someone who’s been there beats all the science. I tracked down a few IVF moms online (anonymously, of course) to see what they went through:
- Jess, 34: “I stopped at 8 weeks after my FET. I was terrified, but my doc said my levels were fine. No issues—my girl’s 2 now!”
- Maria, 29: “I had spotting at 6 weeks, so they kept me on progesterone till 12. It was a pain, but I’d do it again for my twins.”
- Sam, 37: “Missed a shot at 5 weeks by accident. Freaked out, but my ultrasound was perfect. Guess I got lucky.”
These stories show it’s not all black-and-white. Your journey’s unique, but you’re not alone in the ups and downs.
Let’s Vote: What’s Your Plan?
Here’s a fun one—cast your vote:
- I’ll stop progesterone when my doctor says it’s cool.
- I’m sticking with it till 12 weeks, just to be safe.
- I’m too nervous to stop—give me all the progesterone!
Drop your pick in your head (or tell a friend!), and see where you land.
Busting Myths About Progesterone and Miscarriage
There’s a lot of noise out there about progesterone. Let’s clear up some stuff that might be stressing you out:
- Myth: “Low progesterone always causes miscarriage.”
Truth: Nope. Low levels can be a sign of a pregnancy that’s already struggling, not the cause. If the embryo’s not viable (say, due to genetics), no amount of progesterone will save it. - Myth: “You need progesterone forever in IVF.”
Truth: Not really. Once your placenta’s doing its job (around 7-10 weeks), you’re usually good. Supplements are just a bridge. - Myth: “Stopping progesterone means instant miscarriage.”
Truth: Studies say otherwise. Timing matters, but stopping doesn’t flip a miscarriage switch for most.
What’s the Latest Research Saying?
Science isn’t standing still, and neither should we. Here’s what’s fresh in 2025:
- A big review this year looked at over 4,000 IVF pregnancies. They found no major miscarriage bump when progesterone stopped at 5-7 weeks if the pregnancy was healthy. But they stressed monitoring—don’t just quit cold turkey.
- A small 2024 study tested progesterone blood levels after stopping supplements. Women with levels above 15 ng/mL at 7 weeks did just as well as those who kept taking it. Could this be a new way to decide when to stop? Maybe soon.
- On the flip side, a 2023 paper warned that women with past miscarriages might benefit from staying on progesterone longer—up to 12 weeks—if they’re bleeding early. It’s not a sure thing, but it’s worth noting.
The vibe? Researchers are leaning toward shorter progesterone use for some, but they’re not ready to rewrite the rules yet. Your doc’s still your best guide.
Wrapping It Up: Your Next Move
So, will you miscarry if you stop taking progesterone after IVF? There’s no simple yes or no. For most, stopping between 5-12 weeks seems safe, especially if your pregnancy’s humming along. But it’s not a solo decision—your doctor’s in the driver’s seat, and your body’s the map.
Here’s what to do next:
- Talk to your clinic about your stop date. Ask why they picked it and what signs they’re watching.
- Keep an eye on how you feel—spotting or cramps aren’t just annoyances, they’re clues.
- Trust yourself. If stopping freaks you out, ask about tapering or staying on a bit longer. Peace of mind matters.
You’re not just a number in a study—you’re you, and your pregnancy’s one-of-a-kind. Progesterone’s a tool, not a magic wand, but with the right plan, you’ve got this. Got questions? Your doctor’s a call away, and I bet they’d love to hear from you. What’s your next step?