What Is the Cost of IVF? Your Complete Guide to Understanding the Price Tag
April 30, 2025
What Is Novarel Used for in IVF?
April 30, 2025What Is ICSI IVF? Your Complete Guide to This Game-Changing Fertility Treatment
If you’ve been exploring fertility options, you’ve probably come across terms like IVF and ICSI. They might sound like alphabet soup at first, but they’re actually two of the most powerful tools in modern reproductive medicine. IVF, or in vitro fertilization, is the process of fertilizing an egg with sperm outside the body, while ICSI—intracytoplasmic sperm injection—takes it a step further by injecting a single sperm directly into an egg. Together, they form a dynamic duo that’s helped millions of people build families, even when the odds seemed stacked against them.
But what exactly is ICSI IVF? How does it work, who’s it for, and what can you expect if you’re considering it? This guide is here to break it all down in a way that’s easy to digest, with a sprinkle of real-world insight and the latest info to help you feel confident about your next steps. Whether you’re just curious or seriously weighing your options, stick around—there’s a lot to unpack, and we’re diving deep!
Understanding the Basics: IVF Meets ICSI
IVF has been a household name in fertility circles since the first “test-tube baby” was born in 1978. It’s a process where eggs are retrieved from the ovaries, mixed with sperm in a lab dish, and left to fertilize naturally. If all goes well, the resulting embryos are transferred back into the uterus, hoping one sticks around for the long haul—nine months, to be exact.
ICSI, on the other hand, is like IVF’s precision-driven cousin. Introduced in 1992, it was designed to tackle tough cases where sperm couldn’t quite seal the deal on their own. Instead of letting sperm and egg figure things out in a dish, an embryologist picks one healthy-looking sperm and injects it straight into the egg using a tiny needle. It’s a bit like giving nature a gentle nudge—or a firm push, depending on how you look at it.
When we talk about “ICSI IVF,” we mean using ICSI as the fertilization method within the broader IVF process. It’s not a standalone treatment but a turbo-charged upgrade to traditional IVF, tailored for specific challenges. Think of it as a custom job: same car (IVF), but with a souped-up engine (ICSI) for those trickier roads.
Why Pair ICSI with IVF?
So why not just stick with regular IVF? Well, sometimes the sperm needs a little extra help to get the job done. ICSI was originally created for male infertility issues—like low sperm count or poor swimmers—but it’s since become a go-to for other situations too. It’s all about boosting the chances of fertilization when the usual “meet and greet” in the lab dish isn’t cutting it.
Here’s a quick rundown of how they compare:
- Traditional IVF: Sperm and egg mingle in a dish; fertilization happens if a sperm penetrates the egg naturally.
- ICSI IVF: One sperm is hand-picked and injected into the egg, skipping the natural penetration step.
The result? ICSI IVF can turn a “maybe” into a “yes” for couples who might otherwise hit a dead end.
Who Needs ICSI IVF? Is It Right for You?
Not everyone going through IVF needs ICSI—it’s not a one-size-fits-all deal. But it’s a game-changer for certain folks. So, who’s it for? Let’s break it down.
When Sperm Is the Sticking Point
ICSI shines brightest when male infertility is in the picture. If the guy’s sperm isn’t up to par, ICSI can step in to save the day. Here are some common scenarios where it’s a top pick:
- Low Sperm Count: When there aren’t enough sperm to go around, ICSI ensures the best one gets a shot.
- Poor Sperm Motility: If the sperm can’t swim well, they won’t reach the egg on their own. ICSI delivers them right to the doorstep.
- Abnormal Sperm Shape: Weirdly shaped sperm might struggle to break into the egg. ICSI bypasses that hurdle.
- Surgically Retrieved Sperm: For men with blockages or no sperm in their ejaculate (azoospermia), sperm can be pulled from the testicles or epididymis. ICSI makes it usable.
Real talk: About 1 in 6 couples deal with infertility, and half the time, it’s tied to male factors. ICSI has been a lifeline for those cases, turning what used to be a “sorry, we can’t help” into a real chance at parenthood.
Beyond Male Infertility
Here’s where it gets interesting—ICSI isn’t just for guys anymore. Clinics sometimes recommend it for other reasons, even when sperm looks fine. These include:
- Previous IVF Failures: If traditional IVF didn’t result in fertilized eggs, ICSI might up the odds next time.
- Frozen Eggs or Sperm: Thawed samples can be less lively, so ICSI gives them a boost.
- Older Age: For women over 35, egg quality can dip, and ICSI might improve fertilization rates.
- Unexplained Infertility: When no one knows why conception isn’t happening, ICSI can be a troubleshooting tool.
Fun fact: By 2025, over 60% of IVF cycles in the U.S. use ICSI, even in cases without male issues. It’s become a popular safety net, though some experts debate if it’s overused. More on that later!
Quick Quiz: Could ICSI IVF Be for You?
Take a sec to think about your situation. Answer these with a quick yes or no:
- Does your partner have a low sperm count or motility issues?
- Have you tried IVF before without success?
- Are you using frozen eggs or sperm?
- Are you over 35 and worried about egg quality?
If you nodded to any of these, ICSI IVF might be worth a chat with your doctor. It’s not a magic bullet, but it could be the tweak your journey needs.
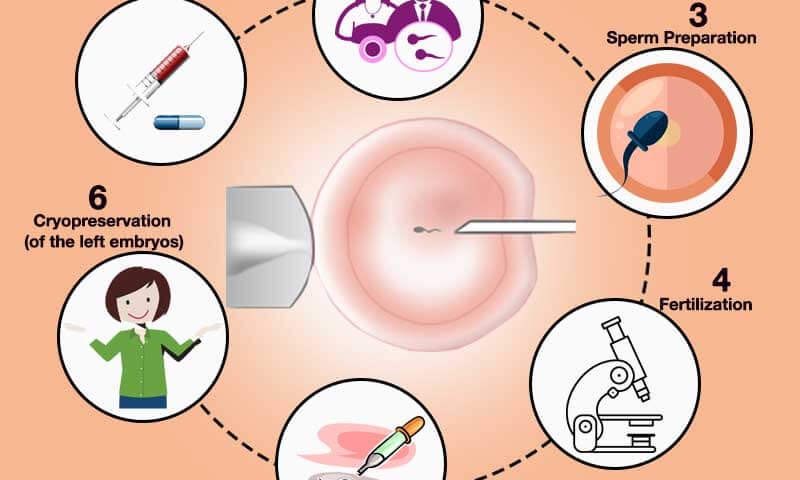
How Does ICSI IVF Work? A Step-by-Step Look
Curious about what goes down in the lab? The ICSI IVF process is a mix of high-tech wizardry and careful timing. Here’s how it unfolds, step by step.
Step 1: Egg Prep
First, the woman takes fertility meds for about 10-14 days to rev up her ovaries. These hormones coax multiple eggs to mature—more eggs mean more chances. When they’re ready, a doctor retrieves them using a thin needle guided by ultrasound. It’s quick, usually 20-30 minutes, and done under light sedation.
Step 2: Sperm Collection
Meanwhile, the guy provides a sperm sample. If that’s not an option (say, due to a blockage), sperm might be surgically extracted from the testicles or epididymis. Either way, the embryologist picks the healthiest-looking sperm under a microscope—think of it like a talent scout spotting the MVP.
Step 3: The Big Moment—Injection
This is where ICSI steals the show. Using a super-fine needle, the embryologist injects one sperm directly into an egg’s cytoplasm (the gooey center). It’s a delicate dance, done under a high-powered microscope. Typically, they’ll do this for multiple eggs to maximize your odds.
Step 4: Embryo Growth
Fertilized eggs—now embryos—chill in an incubator for 3-5 days. The team watches them grow, checking for signs they’re healthy and dividing properly. By day 5, the best ones (blastocysts) are ready for action.
Step 5: Transfer Time
One or two top-notch embryos are transferred into the uterus using a thin catheter. It’s a simple procedure, like a Pap smear, and takes just a few minutes. Any extras can be frozen for later.
Step 6: The Waiting Game
Now, you wait about 10-14 days for a pregnancy test. It’s the longest two weeks ever, but it’s when the magic (hopefully) happens.
Here’s a handy timeline:
| Step | Timeframe | What Happens |
|---|---|---|
| Egg Stimulation | 10-14 days | Hormones boost egg production |
| Egg Retrieval | 20-30 minutes | Eggs collected via needle |
| Sperm Collection | Same day | Sperm gathered or extracted |
| ICSI Fertilization | 1 day | Sperm injected into eggs |
| Embryo Culture | 3-5 days | Embryos grow in the lab |
| Embryo Transfer | 5-10 minutes | Embryos placed in uterus |
| Pregnancy Test | 10-14 days later | Fingers crossed! |
Success Rates: What Can You Expect?
Let’s talk numbers—because when you’re investing time, money, and emotions, you want to know the odds. ICSI IVF boasts impressive fertilization rates, often hitting 50-80% per egg injected. That’s a big win compared to traditional IVF, where fertilization might hover around 50% or less, especially with sperm issues.
But here’s the catch: fertilization isn’t the same as a baby in your arms. Pregnancy and live birth rates depend on a ton of factors—age, egg quality, embryo health, and even luck. Here’s a snapshot based on 2023 data from the Society for Assisted Reproductive Technology (SART):
- Under 35: 40-50% live birth rate per cycle
- 35-37: 30-40%
- 38-40: 20-30%
- Over 40: 10-15%
ICSI doesn’t magically boost these numbers beyond traditional IVF—it’s about getting to fertilization. After that, it’s up to the embryos and your body. Still, for couples with male infertility, ICSI often makes the difference between zero fertilized eggs and a fighting chance.
What Boosts Your Odds?
Want to tilt the scales in your favor? Try these:
- ✔️ Healthy Lifestyle: Eat well, exercise, and skip the smokes—studies show it can improve sperm and egg quality.
- ✔️ Top-Notch Clinic: Pick a place with high success rates and experienced embryologists.
- ❌ Stress Overload: Easier said than done, but stress can mess with hormones. Yoga or a good Netflix binge might help.
The Cost Factor: What’s the Price Tag?
ICSI IVF isn’t cheap—let’s get that out there. In the U.S., a single IVF cycle averages $12,000-$15,000, and adding ICSI tacks on another $1,000-$2,000. That’s just the base price—meds, testing, and extras can push it to $20,000 or more.
Here’s a rough breakdown:
- IVF Base Cost: $12,000
- ICSI Add-On: $1,500
- Medications: $3,000-$5,000
- Freezing Embryos: $1,000 + storage fees
Insurance coverage varies wildly. Some states mandate fertility coverage, but most don’t include ICSI unless it’s medically necessary (like severe male infertility). Globally, costs differ—think $5,000-$10,000 in places like India or Spain, often with similar success rates.
Money-Saving Tips
- ✔️ Shop Around: Compare clinics—some offer package deals or financing.
- ✔️ Grants: Look into fertility grants or nonprofits like BabyQuest.
- ❌ Skipping Consults: Don’t cut corners on initial evaluations; they can save you from failed cycles.
Risks and Realities: What’s the Catch?
No treatment’s perfect, and ICSI IVF has its quirks. Most risks mirror regular IVF, but ICSI adds a few twists.
Common Concerns
- Multiple Births: Transferring more than one embryo ups the chance of twins (or more), which can mean preterm birth risks.
- Ovarian Hyperstimulation: Meds can overstimulate ovaries, causing discomfort or, rarely, serious issues.
- Egg Damage: The injection process might harm some eggs—about 5-10% don’t survive.
The Big Debate: Birth Defects
Here’s where it gets murky. Some studies suggest a slightly higher risk of birth defects with ICSI (3-4% vs. 2-3% in natural conception), especially chromosomal issues. A 2023 review in Human Reproduction found a small uptick in sex chromosome abnormalities, possibly tied to the sperm used rather than ICSI itself. But here’s the kicker: most kids born via ICSI are healthy, and long-term studies (think 30+ years of data) show no major developmental differences.
Underexplored Angle: Emotional Toll
One thing you won’t find in every article? The emotional rollercoaster. ICSI IVF can feel like a pressure cooker—every step’s a milestone, and every setback stings. A 2024 survey by Fertility Network found 70% of patients felt “overwhelmed” by the process. It’s not just physical; it’s a mental marathon too.
Coping Tip: Build a support squad—friends, a therapist, or online forums. You’re not alone, even if it feels that way at 3 a.m.
Fresh vs. Frozen: A New Twist
Here’s a hot topic that’s buzzing in 2025: fresh vs. frozen embryo transfers. Most ICSI IVF articles gloss over this, but it’s worth a look. Fresh transfers happen right after egg retrieval, while frozen ones wait—sometimes months—using cryopreserved embryos.
Recent research leans toward frozen. A 2024 study in Fertility and Sterility found frozen transfers had a 5-10% higher success rate, possibly because the uterus gets a break from hormone overload. Plus, freezing lets you test embryos for genetic issues (PGT-A), weeding out duds.
Fresh vs. Frozen: Pros and Cons
| Approach | Pros | Cons |
|---|---|---|
| Fresh | Faster process, less waiting | Hormones might affect uterus |
| Frozen | Higher success, genetic testing | Extra cost, longer timeline |
Your Move: Ask your doc about your odds with each. It’s not one-size-fits-all—your age, egg count, and sperm quality play a role.
The Sperm Selection Puzzle: Quality Over Quantity
ICSI’s superpower is picking one sperm, but how do they choose? Most clinics use basic visuals—size, shape, wiggle. But here’s a curveball not every article digs into: advanced sperm selection. Techniques like IMSI (super-high magnification) or PICSI (sperm-binding tests) aim to nab the cream of the crop.
A 2023 trial in Reproductive BioMedicine Online showed IMSI bumped fertilization rates by 10% in tough cases. It’s not standard yet—cost and availability are hurdles—but it’s a peek at where ICSI’s headed.
DIY Sperm Boosters
While the lab’s got the fancy tools, guys can help too:
- ✔️ Zinc and Folate: Studies link these to better sperm DNA.
- ✔️ Cool It: Skip hot tubs—heat’s a sperm killer.
- ❌ Tight Jeans: Give the boys some breathing room.
Real Stories: ICSI IVF in Action
Numbers are great, but stories hit home. Meet Sarah and Mike (names changed), a couple from Ohio. Mike had a vasectomy years ago, so sperm had to be surgically retrieved. Traditional IVF wasn’t an option—too few sperm. Enter ICSI. After one cycle, they got three embryos, transferred one, and welcomed a daughter in 2024. “It felt like a miracle,” Sarah says. “ICSI was our bridge.”
Then there’s Priya, 38, from California. No male issues, but two IVF flops left her stumped. Her clinic suggested ICSI to rule out fertilization hiccups. Third time’s the charm—she’s due in July 2025. “I wish I’d known sooner it wasn’t just about sperm,” she says.
These aren’t outliers—ICSI’s opened doors for all kinds of families.
The Overuse Question: Is ICSI Too Popular?
Here’s a spicy take you won’t see everywhere: some experts think ICSI’s overdone. It’s used in over half of IVF cycles, even when sperm’s fine. Why? Clinics say it’s insurance against fertilization failure. Critics argue it’s a cash grab—extra cost, no extra benefit.
A 2024 study in Nature Reviews Urology found no live birth boost from ICSI in non-male factor cases. So, if your sperm’s A-OK, should you skip it? Maybe. It’s a convo worth having with your doc—don’t just nod along.
Poll Time: What’s Your Take?
What do you think about ICSI’s rise? Vote below and see where you stand:
- A) It’s a lifesaver—use it whenever!
- B) Only for male issues, please.
- C) I’m not sure—need more info.
Check back next week for results!
The Future of ICSI IVF: What’s Next?
ICSI’s not standing still. Researchers are tinkering to make it sharper, safer, and more accessible. Here’s what’s cooking:
- AI Sperm Pickers: Algorithms might soon outsmart human eyes, spotting top sperm faster.
- Cheaper Tech: Portable ICSI kits could slash costs, especially in developing countries.
- Sperm DNA Tests: Checking sperm DNA before injection might cut miscarriage risks.
A 2025 pilot study from xAI (yep, the tech folks) showed AI-assisted ICSI hit 85% fertilization—promising stuff! Stay tuned; the next decade could redefine this field.
Your Action Plan: Getting Started
Ready to explore ICSI IVF? Here’s your roadmap:
- Find a Clinic: Look for high success rates and ICSI experience—check SART stats online.
- Ask Questions: Grill your doc on why ICSI’s right (or not) for you.
- Prep Together: Both partners can tweak diet, stress, and habits—teamwork makes the dream work.
- Budget Smart: Map out costs and funding options early.
- Lean on Support: Join a group or forum—Reddit’s r/infertility is a goldmine.
Checklist: Before You Dive In
- ✔️ Semen analysis done?
- ✔️ Hormone levels checked?
- ✔️ Clinic tour booked?
- ❌ Rushing in blind—take your time!
Wrapping Up: Your Journey, Your Way
ICSI IVF isn’t just a procedure—it’s a lifeline, a leap of faith, and sometimes a wild ride. It’s turned “impossible” into “possible” for countless families, from Ohio to Mumbai. Whether it’s low sperm counts, tricky eggs, or just bad luck, this combo’s got a knack for cracking tough cases.
But it’s not about the tech alone—it’s about you. Your story, your hopes, your next steps. Maybe ICSI’s your ticket, maybe it’s not. Either way, you’re armed with the full scoop now: how it works, what it costs, and where it’s headed. So, take a breath, talk it over, and trust your gut. You’ve got this.
Got questions? Drop ‘em in the comments—I’m here to chat. Here’s to your family, however it grows!