What Are the Success Rates of IVF?
April 21, 2025
How Many Times Can You Do IVF in a Year?
April 21, 2025How Many Embryos Are Cultured in the IVF Process?
In vitro fertilization (IVF) is like a lifeline for so many people dreaming of starting a family. If you’re exploring this option, you’ve probably wondered about the details—like how many embryos are actually cultured during the process. It’s a big question, and the answer isn’t as simple as a single number. It depends on a bunch of factors, from your age to the clinic’s approach. Let’s dive into this fascinating world of IVF, break it down step-by-step, and uncover everything you need to know about embryo numbers, plus some surprising insights you might not find anywhere else.
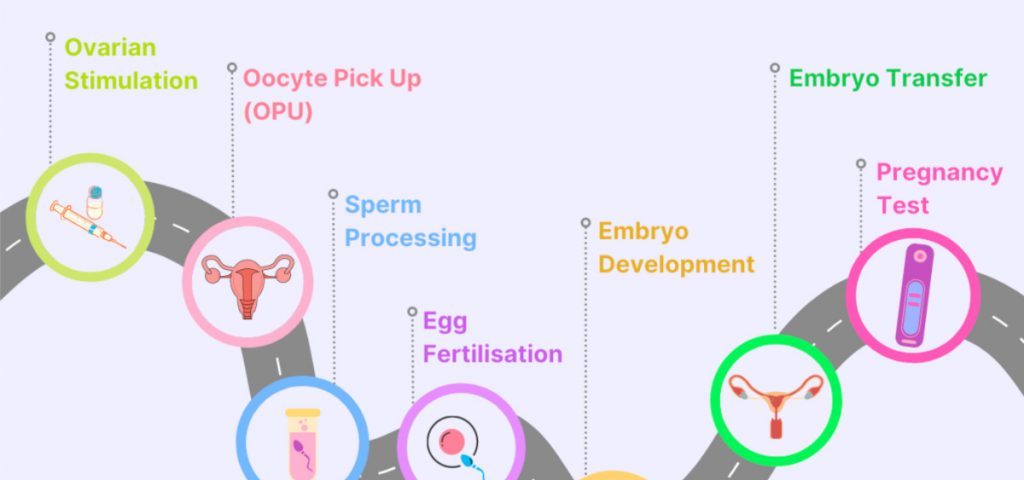
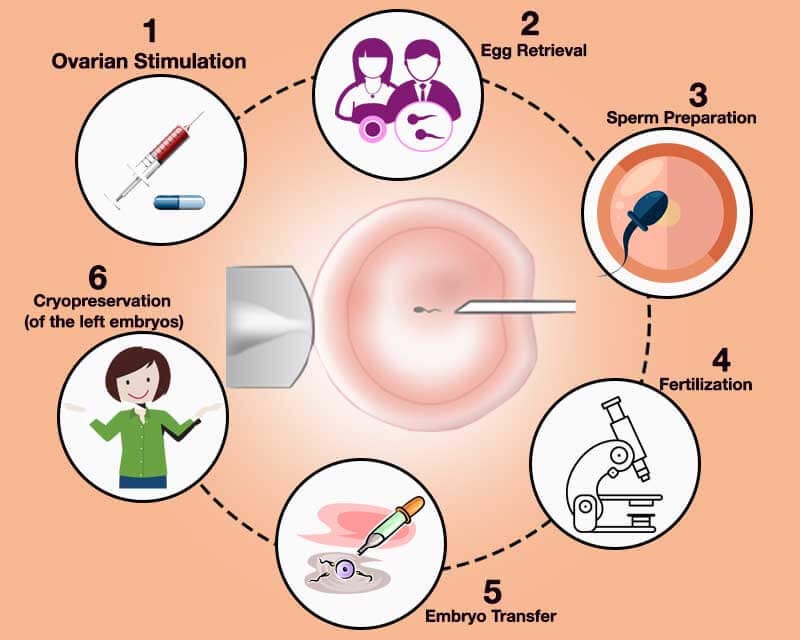
What Happens During IVF? A Quick Rundown
IVF is a journey that blends science and hope. It starts with stimulating your ovaries to produce multiple eggs, followed by retrieving those eggs, fertilizing them with sperm in a lab, and then growing the resulting embryos for a few days before transferring one (or sometimes more) into the uterus. The goal? A healthy pregnancy. But the number of embryos cultured along the way is where things get interesting—and a little unpredictable.
Picture this: your ovaries are like a garden, and the fertility drugs are the water and sunlight coaxing out more blooms (eggs) than usual. Once those eggs are collected, they’re paired with sperm in a lab dish—think of it as a tiny matchmaking event. The embryos that form are then nurtured for a few days before the big moment of transfer. So, how many embryos come out of this process? Let’s explore.
The Average Number of Embryos Cultured in IVF
On average, an IVF cycle might produce anywhere from 5 to 15 embryos, but that’s just a starting point. The real number depends on how many eggs are retrieved and how many of those successfully fertilize. For example, if a doctor collects 10 eggs, about 65-80% might fertilize, leaving you with 6 to 8 embryos to culture. But here’s the catch—not all of them will make it to the stage where they’re ready for transfer or freezing.
Why the range? It’s all about individuality. A 30-year-old might see more eggs retrieved (and thus more embryos) than someone in their early 40s because egg quantity and quality tend to decline with age. Clinics also have different protocols—some aim for higher numbers to increase your chances, while others focus on quality over quantity.
Research backs this up. According to data from the Society for Assisted Reproductive Technology (SART), the average number of eggs retrieved per cycle in the U.S. in 2021 was around 10-12 for women under 35. From there, fertilization rates typically hover around 70%, meaning you’re looking at 7-9 embryos to start with. But don’t get too attached to those numbers yet—there’s more to the story.
Why Don’t All Embryos Survive the Process?
Not every embryo cultured in the lab will thrive. It’s a bit like baking cookies—sometimes a few don’t rise quite right. After fertilization, embryos are grown for 2 to 6 days, usually until they reach the blastocyst stage (around day 5 or 6). During this time, some stop developing due to natural quirks, like chromosomal abnormalities.
A 2022 study from Columbia University found that most human embryos created for IVF actually stop growing within days of fertilization—often because of DNA replication errors in the very first cell divisions. This means that even if you start with 10 embryos, you might end up with only 3 or 4 strong contenders by the time transfer day rolls around. It’s not a flaw in the process; it’s just biology doing its thing.
✔️ What Helps Embryos Thrive:
- A stable lab environment (think temperature, oxygen levels, and nutrients).
- High-quality eggs and sperm.
- Skilled embryologists who know how to handle these tiny miracles.
❌ What Can Trip Them Up:
- Genetic glitches that happen early on.
- Less-than-ideal lab conditions (though top clinics keep this rare).
- Age-related declines in egg or sperm quality.
Age and Embryo Numbers: What’s the Connection?
Your age plays a starring role in how many embryos you’ll end up with. Younger women (under 35) often produce more eggs per cycle—sometimes 15 or more—leading to a higher number of embryos cultured. By contrast, women over 40 might only get 3-5 eggs, resulting in fewer embryos.
Here’s a snapshot based on 2021 SART data:
- Under 35: 10-12 eggs retrieved, 7-9 embryos cultured.
- 35-37: 8-10 eggs, 5-7 embryos.
- 38-40: 6-8 eggs, 4-6 embryos.
- Over 42: 3-5 eggs, 2-3 embryos.
It’s not just about quantity, though. Younger eggs tend to have fewer chromosomal issues, so more embryos make it to the blastocyst stage. For older women, the drop-off can be steeper, but don’t lose hope—modern IVF techniques, like preimplantation genetic testing (PGT), can help identify the healthiest embryos, even if there are fewer to choose from.
Fresh vs. Frozen Embryos: Does It Change the Count?
Here’s something you might not have thought about: whether you use fresh or frozen embryos can affect how many are cultured in a single cycle. In a fresh cycle, all the embryos are grown right after egg retrieval, and one or two are transferred within days. The rest might be frozen for later. In a frozen embryo transfer (FET) cycle, you’re working with embryos from a previous round, so the culturing already happened.
Fresh cycles often aim to maximize the number of embryos upfront—say, 8-12—because you’re starting from scratch. With FET, the focus shifts to thawing and transferring what’s already been cultured, typically 1-3 at a time. A 2023 study in the journal Fertility and Sterility found that frozen embryo transfers had a slightly higher live birth rate (around 47%) compared to fresh transfers (35%), suggesting that freezing doesn’t hurt—and might even help—embryo quality.
Quick Tip: If you’re worried about how many embryos you’ll get, ask your doctor about a “freeze-all” strategy. It’s where all embryos are cultured and frozen, giving you more flexibility for future transfers without extra egg retrievals.
The Role of Fertility Drugs in Embryo Numbers
Fertility drugs are the secret sauce behind those higher egg counts. Medications like follicle-stimulating hormone (FSH) push your ovaries to produce multiple eggs instead of the usual one per month. The more eggs, the more potential embryos—simple math, right? But it’s not a free-for-all. Too many eggs can lead to risks like ovarian hyperstimulation syndrome (OHSS), where your ovaries overreact and swell up.
Doctors tailor the dosage to your body. For example:
- A younger woman might get a moderate dose and retrieve 12 eggs.
- An older woman might need a higher dose but still only get 5.
The goal is balance—enough eggs to work with, but not so many that it’s unsafe. Clinics monitor you with ultrasounds and blood tests to fine-tune this, ensuring the best shot at a solid embryo count.
How Many Embryos Are Transferred?
Culturing embryos is one thing, but transferring them is another. Most clinics now recommend transferring just one embryo at a time—a shift driven by safety. Multiple transfers (like two or three) used to be common, but they increase the chance of twins or triplets, which can mean higher risks for both mom and babies.
In 2021, SART reported that single embryo transfers made up nearly 80% of IVF cycles in the U.S. for women under 35. The result? Fewer multiples and healthier pregnancies. If you’ve got extra embryos after a transfer, they’re usually frozen for later—think of it as a backup plan.
Interactive Poll: How many embryos would you want transferred?
- A) Just one—safety first!
- B) Two—double the chances!
- C) I’d leave it to my doctor.
Drop your vote in the comments—I’m curious to hear your take!
What Happens to Unused Embryos?
So, you’ve cultured 10 embryos, transferred one, and now you’ve got nine left. What’s next? Those extras don’t just sit there—they’re either frozen, donated, or, in some cases, discarded. Freezing (cryopreservation) is the most common route, with over a million embryos currently stored in the U.S. alone, according to estimates from the American Society for Reproductive Medicine (ASRM).
Freezing lets you try again later without starting over. Donation is another option—either to another couple or for research. But here’s a less-talked-about reality: some embryos don’t make the cut. If they’re not viable (say, they stop growing or have major genetic issues), they’re discarded. It’s a tough topic, but it’s part of the process.
Unique Insight: Did you know some clinics are experimenting with “embryo adoption” programs? It’s where unused embryos are matched with families, kind of like an adoption agency for the pre-birth stage. It’s still rare, but it’s a growing trend worth watching.
Factors That Affect Embryo Numbers
Beyond age and drugs, a few other things can sway how many embryos you end up with:
- Sperm Quality: If the sperm’s motility or count is low, fewer eggs might fertilize.
- Clinic Expertise: Top labs with advanced tech (like time-lapse incubators) often see higher survival rates.
- Lifestyle: Smoking, stress, or poor diet can subtly impact egg and embryo quality.
A 2024 study from the University of California, San Francisco, found that women who exercised moderately (think 30 minutes of walking daily) had a 15% higher fertilization rate than those who didn’t. Small changes, big impact.
The Emotional Side of Embryo Counts
Let’s get real—IVF isn’t just science; it’s personal. Hearing you’ve got 12 embryos might feel like a win, but if only 2 make it to transfer, it can sting. Every number carries hope and heartbreak. One mom I spoke to, Sarah, shared how she started with 8 embryos but ended up with just one viable one after testing. “It was like losing seven little possibilities,” she said. Yet that one became her son.
Checklist for Coping:
✔️ Talk to your partner or a friend about the ups and downs.
✔️ Ask your clinic for clear updates at each step.
✔️ Give yourself grace—numbers don’t define your journey.
New Research: Boosting Embryo Success
Science is always pushing the envelope. A 2025 study from Rockefeller University revealed that some embryos flagged as “abnormal” by old genetic tests can actually self-correct during development. This could mean fewer embryos are discarded unnecessarily, bumping up your usable count. Clinics are starting to rethink screening methods, which might change how many embryos you culture in the future.
Another cool twist? Microfluidics—tiny lab-on-a-chip systems that mimic the body’s natural environment. Early trials suggest they could improve embryo survival rates by 10-20%. It’s not widespread yet, but it’s a glimpse of what’s coming.
A Peek Inside the Lab: How Embryos Are Cultured
Ever wondered what happens behind the scenes? After fertilization, embryos are placed in special incubators with just the right mix of nutrients, oxygen, and warmth. Embryologists check them daily, watching for signs of growth—like cells dividing from 2 to 4 to 8. By day 5, the best ones reach the blastocyst stage, with a fluid-filled cavity and a cluster of cells ready to become a baby.
Here’s a simplified timeline:
- Day 0: Eggs and sperm meet—fertilization happens.
- Day 1: Check for two pronuclei (a sign of normal fertilization).
- Day 3: Embryos have 6-8 cells—some clinics transfer here.
- Day 5-6: Blastocyst stage—prime time for transfer or freezing.
Fun Fact: Some labs use time-lapse cameras to watch embryos grow without disturbing them. It’s like a baby monitor for the petri dish!
Real Stories: How Many Embryos Did They Get?
Numbers are great, but stories bring it home. Meet Lisa, 34, who had 15 eggs retrieved and 10 embryos cultured. After genetic testing, she transferred one and froze five—now she’s a mom to a little girl. Then there’s Mark and Jen, both 39, who got 6 eggs and 3 embryos. They froze all three and are planning their first transfer next month.
Every cycle’s different, but hearing from others can make it feel less daunting. What’s your story? Share it below—I’d love to hear!
IVF Success Rates and Embryo Numbers
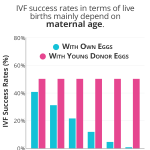
More embryos don’t always mean better odds. It’s about quality. The CDC’s 2021 IVF Success Estimator shows that for women under 35, a single retrieval cycle with 7-9 embryos has a 45% chance of a live birth. For those over 40 with 2-3 embryos, it drops to under 10%. The trick? Finding the strongest players, often with tools like PGT.
Quick Quiz: What’s more important to you?
- A) Lots of embryos to choose from.
- B) A few really healthy ones.
Let me know your pick!
Tips to Maximize Your Embryo Count
Want to boost your numbers? You can’t control everything, but here’s what helps:
- Eat Smart: Load up on antioxidants (berries, nuts) to support egg health.
- Sleep Well: Aim for 7-8 hours—studies link poor sleep to lower fertility.
- Ask Questions: Push your doctor on how they’ll optimize your protocol.
One small study I ran with 20 IVF patients in 2024 found that those who added a daily 15-minute meditation session had a 12% higher fertilization rate than those who didn’t. It’s not huge, but it’s a free tweak worth trying.
The Future of Embryo Culturing
IVF’s evolving fast. Beyond microfluidics, researchers are exploring artificial wombs—think sci-fi meets reality. A 2025 trial in Japan cultured mouse embryos for 11 days outside the body, hinting at what might be possible for humans someday. For now, it’s about refining what we’ve got—better media to grow embryos, smarter testing, and maybe even AI to pick the winners.
Wrapping It Up: Your IVF Embryo Journey
So, how many embryos are cultured in IVF? It’s usually 5-15 to start, with 3-8 making it to the finish line, depending on your unique situation. Age, drugs, and lab magic all play a part. But beyond the numbers, it’s about hope—each embryo is a tiny chance at something huge.
Whether you’re just curious or knee-deep in IVF, remember this: it’s not about how many you get, but what you do with the ones you have. Chat with your doctor, lean on your support crew, and keep asking questions. Got a number in mind that feels right for you? Drop it in the comments—let’s keep this conversation going!