What Is Precycle Screening for IVF?
April 22, 2025
How Much Does an IVF Procedure Cost? Your Guide to Understanding the Price Tag
April 23, 2025Which Is Associated with IVF-ET? Exploring the World of In Vitro Fertilization and Embryo Transfer
In vitro fertilization and embryo transfer (IVF-ET) is a life-changing journey for many people dreaming of starting a family. If you’ve heard the term but aren’t quite sure what it involves—or what’s connected to it—you’re in the right place. This isn’t just about the science; it’s about the real experiences, the emotions, and the little details that make IVF-ET such a unique process. Whether you’re considering it yourself, supporting a loved one, or just curious, let’s dive into what’s associated with this incredible fertility treatment.
IVF-ET isn’t a one-size-fits-all solution. It’s a blend of cutting-edge technology, personal hopes, and sometimes unexpected twists. From the steps of the procedure to the factors that influence success, there’s a lot to unpack. Plus, with new research and trends popping up, there’s always something fresh to explore. So, grab a cozy drink, settle in, and let’s walk through this together.
What Exactly Is IVF-ET?
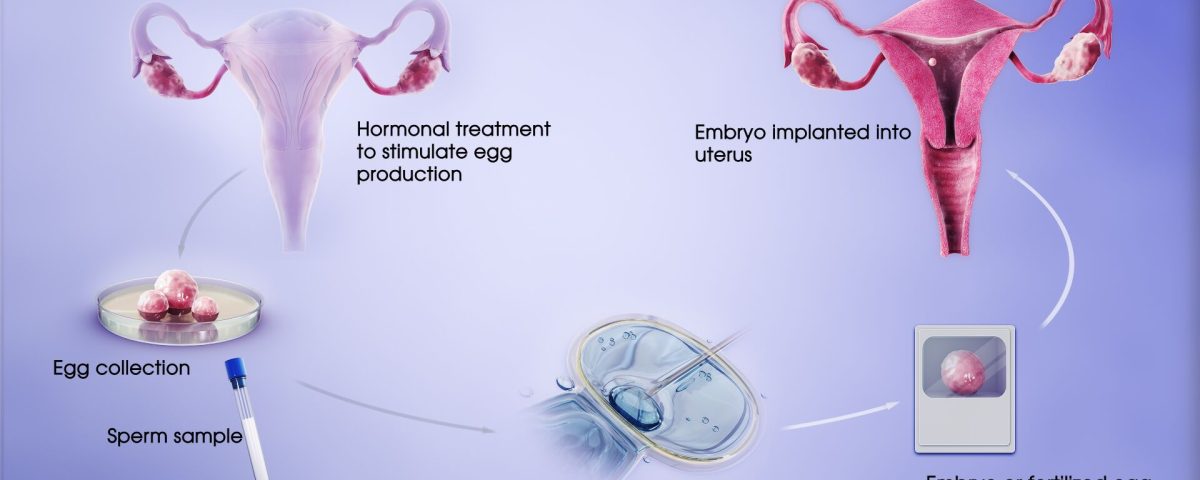
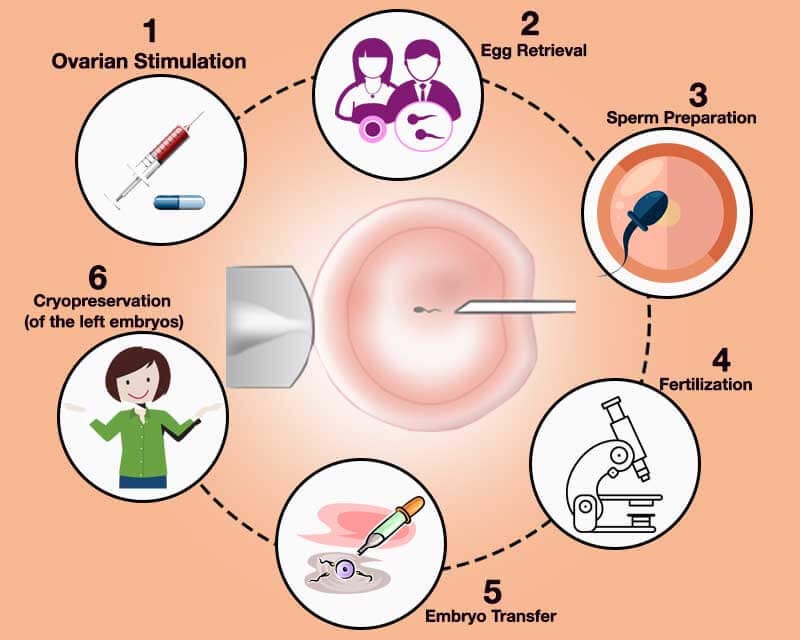
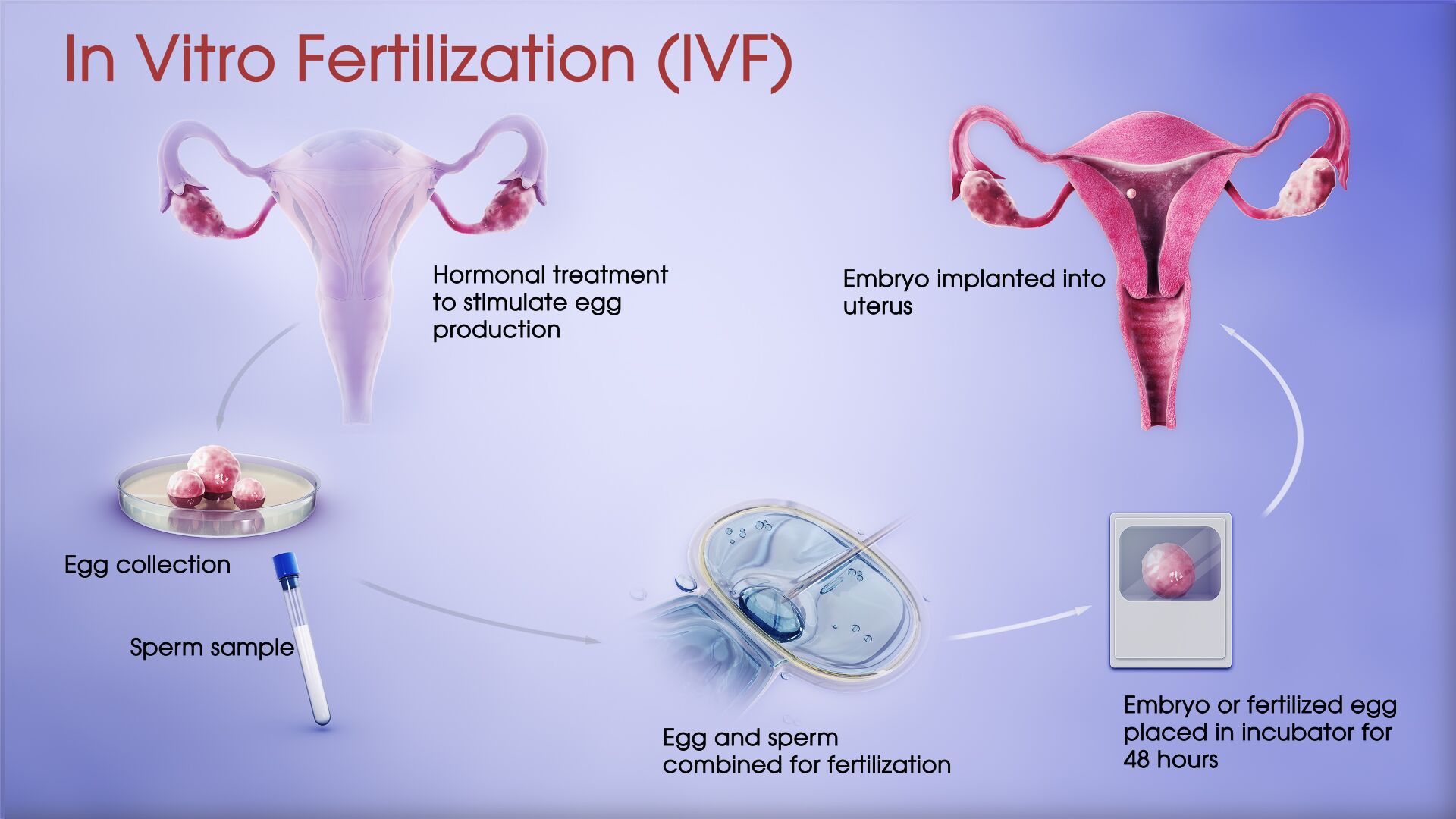
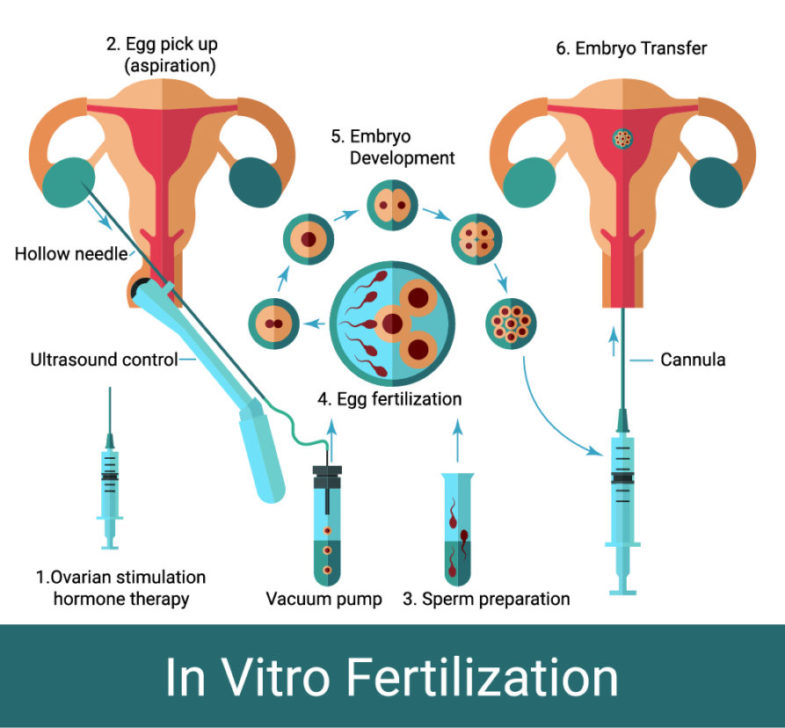
IVF-ET stands for in vitro fertilization and embryo transfer. In simple terms, it’s a process where doctors help create an embryo outside the body (in a lab) and then place it into the uterus to hopefully grow into a baby. “In vitro” means “in glass,” referring to the lab dish where the magic begins, while “embryo transfer” is the step where that tiny embryo gets a new home in the womb.
The process starts with stimulating the ovaries to produce multiple eggs, retrieving those eggs, fertilizing them with sperm, and then growing the embryos for a few days. Once they’re ready, one (or sometimes more) is transferred to the uterus. It’s a team effort between you, your doctor, and a lab full of experts.
But IVF-ET isn’t just about the steps—it’s tied to so much more. Emotions, lifestyle choices, and even the latest tech all play a role. Let’s break it down piece by piece.
The Emotional Rollercoaster of IVF-ET
One thing you won’t find in a lab report? The feelings that come with IVF-ET. This journey can be a wild ride, full of hope, stress, and everything in between. For many, it’s a mix of excitement about the possibility of a baby and anxiety over whether it’ll work.
Picture this: You’re waiting for a call from the clinic to hear how many embryos made it. Your heart’s racing, and you’re refreshing your phone every five seconds. That’s the reality for a lot of people. Studies show that about 30-40% of IVF patients experience significant stress or anxiety during the process, according to research from the American Society for Reproductive Medicine. It’s not just about the physical steps—it’s a mental marathon too.
How to Cope
- Talk it out: Whether it’s with a partner, friend, or therapist, sharing your thoughts can lighten the load.
- Set small goals: Celebrate little wins, like finishing a round of shots, instead of focusing only on the end result.
- Take breaks: Step away for a walk or a Netflix binge when it gets overwhelming.
The emotional side isn’t always front and center in articles, but it’s a huge part of what’s associated with IVF-ET. You’re not alone if you feel this way—it’s part of the package.
The Physical Side: What Your Body Goes Through
IVF-ET isn’t a walk in the park physically either. Your body becomes the star of the show, and it’s working overtime. The process starts with hormone injections to boost egg production. These shots can leave you feeling bloated, tired, or even a little moody—like PMS on steroids.
Next comes egg retrieval, a quick procedure where doctors use a needle to collect eggs from your ovaries. It’s done under sedation, so you won’t feel much, but afterward, you might be sore or crampy for a day or two. Then, after the embryo transfer, you’re in the “two-week wait”—a nail-biting time to see if the embryo sticks.
Common Side Effects
✔️ Bloating or mild cramping
✔️ Fatigue from hormone changes
❌ Severe pain (call your doctor if this happens—it’s rare but serious)
❌ Ignoring rest (your body needs it more than ever)
A 2023 study from the Journal of Reproductive Medicine found that about 1 in 5 women experience mild ovarian hyperstimulation syndrome (OHSS) during IVF, where the ovaries overreact to the hormones. It’s usually manageable, but it’s a reminder of how much your body is doing.
Pro Tip
Keep a journal of how you feel each day. It helps you spot patterns and gives your doctor a clearer picture if something’s off.
Success Rates: What’s the Real Deal?
Everyone wants to know: Will IVF-ET work for me? The truth is, success depends on a bunch of factors—age, health, and even luck. According to the CDC’s 2021 data (the latest full report as of April 2025), the live birth rate per IVF cycle is about 31% for women under 35. That drops to 23% for ages 35-37 and 9% for 38-40. Over 40? It’s tougher, but not impossible—around 3-5% with your own eggs.
What’s cool is that frozen embryo transfers (a big part of IVF-ET) are getting better. A 2024 study from Fertility and Sterility showed frozen transfers now have a slightly higher success rate than fresh ones—up to 35% for under-35s. Why? Freezing gives doctors more control over timing, and embryos can be stored until your body’s in peak condition.
What Boosts Your Odds?
- Age: Younger eggs and uteruses tend to do better.
- Lifestyle: Quitting smoking or cutting stress can make a difference.
- Clinic quality: Some places have success rates way above average—check their stats!
Success isn’t guaranteed, but knowing what’s associated with better outcomes can help you feel more in control.
Interactive Quiz: What’s Your IVF-ET Knowledge?
Let’s take a quick break—test your IVF-ET smarts with this mini quiz! Answer in your head or jot it down.
- What does “in vitro” mean?
A) Inside the body
B) In a lab dish
C) During surgery - How long is the typical “two-week wait”?
A) 7 days
B) 10-14 days
C) 3 weeks - What’s one factor that boosts IVF success?
A) Drinking coffee
B) Being under 35
C) Skipping exercise
(Answers: 1-B, 2-B, 3-B) How’d you do? If you aced it, you’re already ahead of the curve!
The Role of Sperm in IVF-ET
IVF-ET isn’t just about eggs—sperm gets equal billing. If sperm quality is low (think slow swimmers or odd shapes), it can affect fertilization. That’s where techniques like intracytoplasmic sperm injection (ICSI) come in. With ICSI, a single sperm is injected right into an egg, skipping the “swim test.” It’s used in about 70% of IVF cycles, per the European Society of Human Reproduction and Embryology.
But here’s something not everyone talks about: Sperm DNA damage. A 2024 study from Reproductive BioMedicine Online found that high DNA fragmentation in sperm can lower embryo quality, even with ICSI. It’s not a dealbreaker, but it’s a hidden factor worth checking.
Sperm Health Tips
- Eat antioxidants: Think berries, nuts, and leafy greens—they fight DNA damage.
- Avoid heat: Hot tubs and tight pants can hurt sperm production.
- Get tested: A simple semen analysis can spot issues early.
Sperm’s role is half the equation, and small changes can tip the scales.
The Tech Behind IVF-ET: What’s New?
IVF-ET isn’t stuck in the past—it’s evolving fast. One hot topic is time-lapse imaging. Clinics use special cameras to watch embryos grow without disturbing them. A 2023 trial from the University of Oxford showed this tech can boost success rates by 5-10% by picking the healthiest embryos.
Then there’s artificial intelligence (AI). Some labs now use AI to analyze embryo quality, predicting which ones are most likely to implant. A 2025 report from Nature Medicine found AI-assisted cycles had a 12% higher pregnancy rate in early tests. It’s not everywhere yet, but it’s a game-changer on the horizon.
What’s Next?
- Gene editing: Still experimental, but it could one day fix genetic issues in embryos.
- Lab-grown eggs: Scientists are working on making eggs from skin cells—wild, right?
Tech is pushing IVF-ET into the future, and it’s exciting to see where it’ll go.

Lifestyle Factors You Didn’t Know Matter
You might not think your daily habits tie into IVF-ET, but they do. Take diet: A 2024 Harvard study found women eating a Mediterranean diet (lots of veggies, fish, and olive oil) had a 20% higher chance of success compared to those on high-sugar diets. It’s not about perfection—it’s about giving your body a solid foundation.
Sleep’s another biggie. Research from the Sleep Research Society in 2023 showed that women getting less than 7 hours a night had lower embryo quality. Why? Hormones like melatonin, which regulate sleep, also help eggs mature.
Quick Lifestyle Checklist
✔️ Eat colorful fruits and veggies daily
✔️ Aim for 7-8 hours of sleep
❌ Cut back on processed snacks
❌ Don’t skip breakfast—it kickstarts your metabolism
These tweaks won’t guarantee a baby, but they’re part of what’s associated with better IVF-ET results.
The Cost Factor: What’s the Price Tag?
IVF-ET isn’t cheap, and that’s a big piece of the puzzle. In the U.S., one cycle averages $12,000-$15,000, not counting meds (another $3,000-$5,000), according to the American Society for Reproductive Medicine. Insurance coverage varies—some states mandate it, others don’t.
Globally, it’s a mixed bag. In the UK, the NHS might cover a cycle if you qualify, but waitlists are long. In places like India or Mexico, costs drop to $3,000-$6,000, sparking “fertility tourism.”
Saving Strategies
- Shop around: Clinics have different prices—compare a few.
- Look for grants: Groups like BabyQuest offer financial help.
- Consider mini-IVF: It uses fewer drugs and costs less, though success rates vary.
Money’s a stressor, but options exist to make it more doable.
Poll: What’s Your Biggest IVF-ET Question?
Let’s get interactive again! If you could ask one thing about IVF-ET, what would it be? Pick one (or share your own in your mind):
- A) How can I boost my chances?
- B) What’s the hardest part?
- C) How do I pick a clinic?
No pressure—just a fun way to think about what matters to you. Most people I’ve chatted with pick A, but every answer’s valid!
The Endometrium: The Unsung Hero
The uterus lining, or endometrium, is like the welcome mat for an embryo. If it’s not thick and sticky enough, the embryo might not implant. Doctors aim for a lining of 7-10 mm before transfer, measured by ultrasound.
A 2024 study from the Journal of Assisted Reproduction and Genetics found that adding endometrial scratching (a light scrape to “wake up” the lining) boosted implantation rates by 15% in women with past failures. It’s not standard yet, but it’s a hot topic.
How to Prep Your Endometrium
- Stay hydrated: Water helps blood flow to the uterus.
- Ask about supplements: Vitamin E or L-arginine might help (check with your doc).
- Relax: Stress can thin the lining—yoga’s a win here.
The endometrium doesn’t get enough love, but it’s a key player in IVF-ET.
Frozen vs. Fresh: Which Is Better?
With IVF-ET, you’ve got two transfer options: fresh or frozen embryos. Fresh means transferring right after fertilization; frozen means storing them for later. Which wins?
Frozen’s pulling ahead. A 2025 meta-analysis from The Lancet showed frozen transfers had a 33% live birth rate versus 28% for fresh in women under 38. Why? Freezing lets your body recover from hormone shots, and doctors can time the transfer perfectly.
Fresh vs. Frozen Breakdown
| Factor | Fresh | Frozen |
|---|---|---|
| Timing | Immediate | Flexible |
| Success Rate | Slightly lower | Slightly higher |
| Cost | One cycle | Extra freezing fees |
| Body Recovery | Less time | More time |
Frozen’s not always the answer—some prefer fresh to avoid delays—but it’s a trend worth watching.
The Social Stigma: Breaking the Silence
IVF-ET comes with a side of judgment sometimes. People might whisper, “Why can’t they just conceive naturally?” or assume it’s “playing God.” It’s outdated thinking, but it stings.
A 2023 survey by Resolve: The National Infertility Association found 1 in 4 IVF patients felt judged by friends or family. Social media’s helping, though—hashtags like #IVFjourney on X show folks sharing stories and building community.
How to Handle It
- Own your story: You don’t owe anyone an explanation.
- Find your crew: Online groups or local meetups can be a lifeline.
- Educate gently: A quick “It’s just science helping nature” can shut down nosy questions.
The stigma’s fading, but it’s still part of the IVF-ET world for now.
Unique Angle: The Partner’s Perspective
Most articles focus on the person carrying the baby, but what about their partner? They’re in the trenches too—mixing shots, holding hands during retrieval, and biting nails during the wait. A 2024 study from Psychology Today found 60% of partners felt “helpless” during IVF-ET, wanting to fix things but not knowing how.
Partner Support Ideas
- Learn the lingo: Know what “follicles” or “blastocyst” mean—it shows you’re in it together.
- Be the cheerleader: A “You’ve got this” can mean the world.
- Take care of you: Partners need breaks too—don’t burn out.
Partners are the unsung heroes, and their role deserves a spotlight.
Mini Case Study: Sarah’s Story
Meet Sarah, a 34-year-old teacher who did IVF-ET in 2024. She and her husband tried for three years before starting. Her first cycle failed—only one embryo, and it didn’t implant. Crushed, she switched clinics, tweaked her diet, and tried acupuncture. Cycle two? Three healthy embryos, one transferred, and now she’s 20 weeks pregnant.
Sarah’s takeaway: “It’s not just luck—it’s persistence and finding what works for you.” Her story’s not rare—about 40% of IVF patients need multiple cycles, per the CDC. It’s a reminder that IVF-ET is a marathon, not a sprint.
The Future of IVF-ET: What’s on the Horizon?
IVF-ET’s not done evolving. Beyond AI and time-lapse, there’s talk of “mini-IVF” for lower costs and gentler hormone doses. A 2025 pilot from Stanford showed it’s got a 25% success rate—lower than standard IVF, but half the price.
Then there’s fertility preservation. More people are freezing eggs or embryos early, even before they’re ready for kids. The American College of Obstetricians and Gynecologists says egg freezing jumped 20% from 2020 to 2024. It’s tied to IVF-ET because those frozen eggs often become part of the process later.
What to Watch
- Affordability: New methods could drop costs.
- Access: Telehealth consults are making IVF-ET reachable for rural folks.
- Ethics: As tech advances, debates about “designer babies” heat up.
The future’s bright—and a little mind-blowing.
Your IVF-ET Action Plan
Ready to dive in or support someone who is? Here’s a step-by-step guide to get started:
- Research clinics: Look at success rates, reviews, and vibes—visit if you can.
- Ask questions: What’s their frozen transfer rate? Do they use AI?
- Prep your body: Start that healthy diet and sleep routine now.
- Build a support net: Line up your people—partner, friends, or a counselor.
- Plan finances: Check insurance, save up, or explore grants.
It’s not overwhelming if you take it one step at a time.
Final Thoughts: IVF-ET Is More Than a Procedure
IVF-ET isn’t just about eggs, sperm, and labs—it’s about hope, resilience, and the little things that make it personal. From the emotional highs and lows to the tech that’s changing the game, it’s a world of its own. Whether it’s the partner’s quiet strength, the endometrium’s sneaky importance, or the cost juggling act, every piece matters.
If you’re on this path, you’re part of something big. It’s not always easy, but it’s always worth exploring. What’s associated with IVF-ET? A whole lot of science, a dash of grit, and a ton of heart. Where will your journey take you?