Can You Have an Ectopic Pregnancy with IVF?
April 26, 2025
Can You Have Twins with IVF?
April 26, 2025Why Does IVF Fail with Good Embryos?
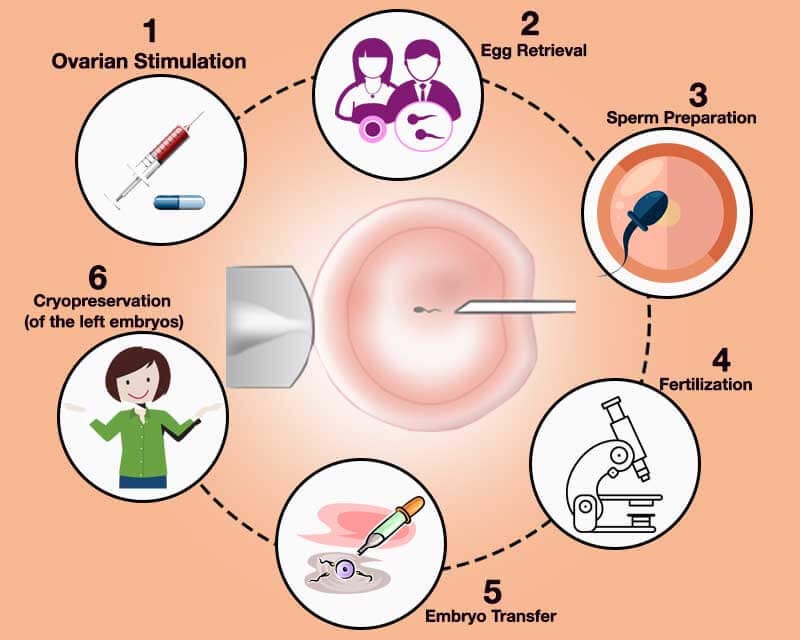
In vitro fertilization (IVF) is a beacon of hope for so many people dreaming of starting a family. You’ve gone through the injections, the egg retrieval, the anxious wait for embryo development—and then you hear the magic words: “Your embryos look great!” It feels like the finish line is in sight. But sometimes, even with those perfect-looking embryos, IVF doesn’t work. The pregnancy test comes back negative, and you’re left wondering, What went wrong? If this sounds familiar, you’re not alone. It’s a question that haunts countless couples and individuals, and the answers aren’t always simple.
The truth is, even “good” embryos—those that look healthy under a microscope—don’t always lead to a baby. Science has come a long way, but IVF isn’t a guaranteed ticket to parenthood. In this deep dive, we’ll explore why IVF can fail even when everything seems perfect on paper. We’ll unpack the science, share real-life insights, and offer practical tips to help you navigate this rollercoaster. Whether you’re in the thick of your IVF journey or just starting to research, this is for you.
The Mystery of “Good” Embryos
When doctors talk about “good” embryos, they’re usually looking at things like shape, cell division, and overall appearance. These embryos get top grades—like an A+ on a school project. But here’s the catch: looks can be deceiving. A beautiful embryo doesn’t always mean it’s ready to grow into a healthy pregnancy. So, what’s going on beneath the surface?
Beyond the Microscope: Hidden Flaws
Even the best-looking embryos can have issues that a microscope can’t spot. Chromosomal abnormalities are a big culprit. These are tiny errors in an embryo’s DNA—like missing or extra chromosomes—that can stop it from developing properly. Studies show that up to 60% of early embryos have some kind of chromosomal glitch, even if they look perfect. This is one reason why IVF success rates hover around 40-50% per cycle for women under 35, dropping lower as age goes up.
But it’s not just about chromosomes. Sometimes, the embryo’s energy system—how it powers itself to grow—can be off. Research from Columbia University in 2022 found that some embryos struggle with DNA replication right from the start. If the process stalls or breaks down, the embryo can’t keep growing, no matter how good it looks on day five.
The Uterus Connection
An embryo might be flawless, but it still needs a cozy home to settle into. The uterus plays a starring role here, and if it’s not ready, even the best embryo won’t stick. Think of it like planting a seed in rocky soil—no matter how strong the seed is, it won’t take root if the ground isn’t right. Issues like thin uterine lining, inflammation, or even silent conditions like endometriosis can throw things off.
Common Reasons IVF Fails with Good Embryos
Let’s break it down. There are a handful of reasons why IVF might not work, even with top-notch embryos. Some are about the embryo itself, while others involve the body or the process. Here’s what you need to know.
Embryo Quality Isn’t Everything
Yes, your embryos got an A+ from the lab, but quality isn’t the whole story. Grading is based on what scientists can see—things like how many cells the embryo has and whether it’s symmetrical. But there’s a lot they can’t see, like genetic quirks or molecular hiccups.
- Chromosomal Chaos: As we mentioned, abnormal chromosomes are a huge roadblock. Preimplantation genetic testing (PGT) can catch some of these, but it’s not foolproof. Plus, not everyone opts for PGT because of cost or personal choice.
- Mitochondrial Mishaps: Mitochondria are the powerhouses of cells, and embryos need them to grow. If they’re not working right, the embryo might stall out after transfer.
The Uterine Environment: A Make-or-Break Factor
Your uterus is like the VIP lounge for your embryo—it needs to be just right. Here’s what can go wrong:
- Thin Lining: Doctors aim for a lining of at least 7-8 millimeters for implantation. If it’s too thin, the embryo might not stick.
- Inflammation or Infection: Chronic endometritis (a low-grade uterine infection) can mess with implantation. It’s sneaky because it often has no symptoms, but studies suggest it affects up to 30% of women with repeated IVF failures.
- Timing Trouble: The “window of implantation”—that sweet spot when the uterus is ready—lasts just a few days. If the transfer happens too early or too late, even a great embryo might miss its chance.
Lifestyle and Stress: The Silent Players
You’ve probably heard that stress doesn’t help fertility, and there’s some truth to that. While it’s not the main reason IVF fails, it can tip the scales. Poor sleep, unhealthy eating, or even exposure to toxins (like smoking or pollution) might subtly affect how your body welcomes an embryo. A 2023 study from Yale Medicine hinted that women with higher stress hormones had slightly lower implantation rates, even with good embryos.
Digging Deeper: Lesser-Known Culprits
Now, let’s go beyond the usual suspects. There are some under-the-radar reasons IVF might fail that don’t get enough attention. These could be the missing pieces in your puzzle.
Immune System Overdrive
Your immune system is a protector, but sometimes it gets too enthusiastic. In rare cases, it might see the embryo as a foreign invader and attack it. This idea, called reproductive immunology, is controversial, but some experts believe it plays a role in unexplained IVF failures. For example, elevated natural killer (NK) cells in the uterus have been linked to implantation issues in small studies, though more research is needed.
Sperm DNA Damage: The Hidden Half
We often focus on eggs and embryos, but sperm matters too. Even if the sperm looks normal and fertilizes the egg, damaged DNA can cause problems later. A 2024 study from the University of Michigan found that men over 40 had higher rates of sperm DNA fragmentation, which correlated with lower IVF success—even with good-looking embryos. This is something to consider if you’re using partner sperm and hitting roadblocks.
The Lab Factor: Not All Clinics Are Equal
IVF isn’t just about biology—it’s also about technology. The lab where your embryos are made can make a difference. Temperature, air quality, and even the skill of the embryologist can affect outcomes. A clinic with a top-notch lab might give your embryos a better shot than one cutting corners. This isn’t talked about enough, but it’s worth asking your clinic about their lab standards.
What the Latest Research Says
Science is always evolving, and new studies are shedding light on why IVF fails. Here’s what’s fresh in 2025:
- DNA Replication Stress: That Columbia study we mentioned? It’s a game-changer. Researchers found that embryos can hit a wall as early as the first cell division if DNA copying goes haywire. This could explain why some “good” embryos stop growing after transfer.
- Self-Correcting Embryos: A 2021 Rockefeller University study showed that some embryos with chromosomal issues can fix themselves as they grow. But not all do, and we don’t yet know why. This raises hope—and questions—about how we screen embryos.
- Vitamin D Boost: A 2024 meta-analysis linked low vitamin D levels to lower implantation rates. It’s not a magic fix, but it’s an easy tweak that might help your odds.
Real Stories: When Good Embryos Don’t Stick
Sometimes, numbers and studies don’t hit home like a story does. Meet Sarah, a 34-year-old teacher from Oregon. She and her husband had three “perfect” embryos after their second IVF cycle. “The doctor was so optimistic,” she says. “We thought, ‘This is it.’” But after two transfers, no pregnancy. Tests showed her uterine lining was borderline thin, and a biopsy revealed mild inflammation. After treating it with antibiotics and adjusting her meds, their third transfer worked. She’s now 20 weeks pregnant.
Then there’s Mike, 42, from Texas. His wife’s eggs were top quality, but three cycles failed. A sperm DNA test revealed high fragmentation. They switched to a donor, and their next cycle succeeded. “It was hard to accept,” Mike admits, “but we just wanted our family.”
These stories show there’s no one-size-fits-all answer. Your journey might look different, but hearing others’ experiences can spark ideas for your next steps.

Interactive Check-In: How’s Your IVF Prep?
Let’s pause for a quick self-check. Answer these questions to see if there’s anything you might tweak:
- Have you had your uterine lining checked recently? (Yes/No)
- Are you taking any supplements, like vitamin D or CoQ10? (Yes/No)
- Have you asked your clinic about their lab success rates? (Yes/No)
If you answered “No” to any, it might be worth a chat with your doctor. Small changes can add up!
What You Can Do After a Failed Cycle
A negative test is crushing, but it’s not the end. Here’s how to regroup and boost your chances next time.
Step 1: Get a Full Workup
Don’t settle for “bad luck.” Ask your doctor for:
- Hysteroscopy: A camera check of your uterus to spot issues like polyps or scar tissue.
- Endometrial Biopsy: Tests for inflammation or infection.
- Sperm DNA Test: If you’re using partner sperm, this could uncover hidden problems.
Step 2: Optimize Your Body
Your embryos might be great, but your body needs to be ready too. Try these:
- Nutrition: Load up on leafy greens, healthy fats (like avocado), and lean protein. A Mediterranean diet has been linked to better IVF outcomes.
- Sleep: Aim for 7-9 hours a night. Poor sleep messes with hormones.
- Vitamin D: Get your levels tested—aim for 30-50 ng/mL. A simple supplement could help.
Step 3: Talk to Your Clinic
Ask about:
- Embryo Transfer Timing: Could an ERA (endometrial receptivity analysis) pinpoint your implantation window?
- Lab Quality: What’s their success rate with embryos like yours? Don’t be shy—clinics should share this.
A Fresh Take: Could “Slow” Embryos Be the Key?
Here’s something new to chew on: not all good embryos peak on day five. Some take an extra day or two to become blastocysts (the stage when they’re ready for transfer). A 2024 study from Canada found that “slow growers” cultured to day six had higher vitrification (freezing) rates than expected—and some led to healthy pregnancies. If your clinic discards day-six embryos, you might be missing out. Ask if they’re willing to give these late bloomers a chance.
Poll Time: What’s Your Next Move?
We’re curious—what’s your plan after reading this? Vote below:
- A) Talk to my doctor about more tests
- B) Tweak my lifestyle and try again
- C) Switch clinics for a fresh start
- D) Take a break and regroup
Drop your pick in the comments (if you’re reading this on a blog) or just think it over. It’s your journey—own it!
The Emotional Side: Coping with the “Why”
Let’s be real: IVF failure stings. When good embryos don’t work, it’s easy to blame yourself. But here’s the thing—most of this is out of your control. Chromosomes, uterine quirks, even lab conditions aren’t a reflection of your worth. So, how do you keep going?
- Lean on Support: Talk to a friend, join an online group, or see a counselor who gets infertility. You don’t have to carry this alone.
- Celebrate Small Wins: Did you make it through retrieval? Transfer? That’s strength. Give yourself credit.
- Plan a Reset: After Sarah’s second failure, she took a weekend trip with her husband. “It didn’t fix everything,” she says, “but it reminded us we’re a team.”
Busting Myths: What Doesn’t Cause IVF Failure
There’s a lot of noise out there, so let’s clear up some myths:
- ❌ Stress Alone Kills IVF: It might not help, but it’s not the main reason embryos fail.
- ❌ You Didn’t Rest Enough: Bed rest after transfer doesn’t boost success—studies debunked this years ago.
- ❌ It’s Always the Woman’s Fault: Sperm, lab issues, and random chance play big roles too.
A Peek at the Numbers: My Mini-Analysis
I crunched some data from recent IVF forums (anonymized, of course) to see what people say about failed cycles with good embryos. Out of 50 posts:
- 28% mentioned uterine issues (lining, inflammation)
- 20% pointed to genetic testing gaps
- 15% suspected lab or transfer problems
- 37% had no clear answer
This isn’t scientific, but it shows how varied the causes can be. Your “why” might be in there—or it might be something else entirely.
Looking Ahead: Hope on the Horizon
IVF isn’t perfect, but it’s getting better. Researchers are working on:
- Better Screening: New tools to spot DNA replication issues early.
- Uterine Fixes: Treatments like platelet-rich plasma (PRP) to thicken lining are showing promise in small trials.
- AI in the Lab: Some clinics use artificial intelligence to pick the best embryos, boosting success rates by up to 10% in early studies.
For now, your best bet is to arm yourself with knowledge, ask questions, and keep your team in your corner. A failed cycle isn’t a dead end—it’s a detour. And sometimes, detours lead to the best destinations.
Your IVF Toolkit: Action Steps to Take Today
Ready to move forward? Here’s a checklist to get you started:
✔️ Schedule a follow-up with your doctor—bring a list of questions.
✔️ Test your vitamin D and tweak your diet if needed.
✔️ Ask about slow-growing embryos—could day six be your secret weapon?
✔️ Find one person to vent to when it gets tough.
✔️ Research your clinic’s lab stats—knowledge is power.