Why Do Republicans Oppose IVF? A Deep Dive into the Debate
April 26, 2025
Can You Have an Ectopic Pregnancy with IVF?
April 26, 2025Why Is IVF Morally Wrong?
In vitro fertilization (IVF) has been a game-changer for many families struggling with infertility. It’s celebrated as a medical marvel that brings hope where there once was none. But beneath the surface of this widely accepted practice lies a web of ethical questions that don’t always make it into the headlines. For some, IVF raises red flags about the value of human life, the natural process of conception, and the unintended consequences of playing with biology. If you’ve ever wondered about the moral side of IVF—or even if you haven’t—this deep dive will walk you through the concerns that make people pause. We’ll explore the big issues, unpack the science, and look at real-life implications, all while keeping it real and relatable.
The Big Picture: What’s at Stake with IVF?
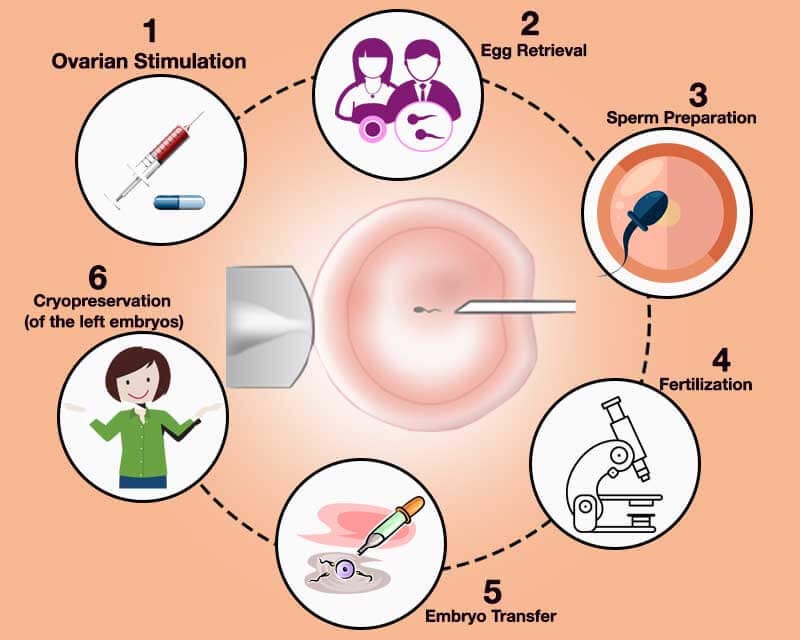
IVF is a process where eggs are taken from a woman’s body, fertilized with sperm in a lab, and then placed back into the womb to grow into a baby. It sounds straightforward, right? But the simplicity ends there. Every year, millions of embryos are created through IVF, and not all of them end up as babies. Some are frozen, some are discarded, and others are used for research. This raises a fundamental question: when does life begin, and what rights do these tiny clusters of cells have?
For many, the moral debate starts with the belief that life begins at conception. If you see an embryo as a human being with potential, the idea of tossing it aside or freezing it indefinitely feels wrong. It’s not just a theoretical issue—real numbers back this up. According to the American Society for Reproductive Medicine, over 1 million embryos are currently frozen in the U.S. alone. That’s a staggering figure when you think about what it means for each one.
But it’s not just about embryos. IVF also challenges how we view family, parenthood, and even the role of technology in our lives. Are we crossing a line by taking conception out of the bedroom and into the lab? Let’s break it down step by step.
The Embryo Dilemma: Life or Just Cells?
One of the biggest sticking points with IVF is what happens to the embryos that don’t get used. In a typical IVF cycle, doctors create multiple embryos to increase the chances of success. Maybe 5 or 10 are made, but only one or two are implanted. So, what happens to the rest?
- Frozen Forever: Many embryos are cryopreserved—frozen in liquid nitrogen—for future use. Sounds practical, but here’s the catch: some stay frozen for years, even decades, with no clear plan. Couples divorce, change their minds, or pass away, leaving these embryos in limbo. A 2023 study from the Guttmacher Institute estimated that up to 20% of frozen embryos are abandoned over time.
- Thrown Away: If they’re not frozen or donated, leftover embryos are often discarded. To some, this feels like throwing away a potential life. It’s not a small number either—research from the National Institutes of Health suggests that tens of thousands of embryos are destroyed annually in the U.S.
- Research Fodder: Some embryos are donated to science, where they’re used to study diseases or develop new treatments. While this might sound noble, it still means the embryo is destroyed in the process, sparking debates about whether it’s ethical to use human life as a lab tool.
Imagine you’re a parent with a freezer full of embryos. What do you do? Keep paying storage fees forever? Donate them to another couple? Let them go? It’s a tough spot, and it’s one that IVF puts people in all the time. For those who believe life starts at fertilization, every one of these options feels like a moral compromise.
What Does Science Say?
Science tells us an embryo has the full genetic makeup of a human from day one. By day five, it’s a blastocyst—a tiny ball of cells with the potential to become a baby. But potential isn’t the same as personhood, right? That’s where the debate gets messy. A 2024 report from the Journal of Medical Ethics found that 60% of Americans think embryos deserve some moral consideration, but only 25% see them as full humans. So, even the public is split on this.
The Natural Connection: Is IVF Too Artificial?
Another angle to consider is how IVF changes the way babies are made. For centuries, conception happened through the intimate act of love between two people. IVF flips that script. It’s a clinical process—eggs and sperm meet in a petri dish, guided by a doctor’s hand, not nature’s rhythm. To some, this feels like a step too far.
Think about it like this: if you bake a cake from scratch, you mix the ingredients yourself, feeling the dough come together. Now imagine a machine does it all for you—same cake, different vibe. IVF is like that machine. The end result might be a baby, but the process lacks the personal, natural connection that many hold sacred.
This isn’t just a romantic notion. Religious groups, like the Catholic Church, argue that separating conception from the marital act undermines the dignity of life. Their stance, outlined in the 1987 document Donum Vitae, says procreation should be a unified act of love, not a lab experiment. Even if you’re not religious, you might wonder: does taking nature out of the equation change how we value the outcome?
A Real-Life Example
Take Sarah and Mike, a couple I heard about through a friend. They tried IVF after years of infertility. It worked—they had a beautiful daughter. But Sarah later said she felt disconnected from the process. “It was like someone else made my baby for me,” she admitted. That sense of detachment isn’t rare, and it’s something IVF clinics don’t always talk about.
The Risks Nobody Talks About
IVF isn’t just a moral puzzle—it’s a physical one too. The process comes with risks that often get glossed over in the excitement of a possible baby. For women, it’s a grueling journey of hormone shots, egg retrieval, and emotional ups and downs. For kids born through IVF, there’s evidence of higher health risks.
- For Moms: Ovarian hyperstimulation syndrome (OHSS) is a real danger, where the ovaries swell painfully from all those hormones. It affects up to 10% of IVF patients, per the Mayo Clinic. Plus, carrying multiples (twins or more) is common with IVF, raising the odds of premature birth or complications.
- For Babies: Studies show IVF babies have a slightly higher chance of birth defects—about 1.5 times more than naturally conceived kids, according to a 2022 study in The Lancet. Preterm birth and low birth weight are also more common, especially with multiples.
Here’s a quick breakdown:
| Risk | IVF Stats | Natural Conception |
|---|---|---|
| Birth Defects | 4-6% | 3-4% |
| Preterm Birth | 12% | 8% |
| Multiple Pregnancies | 20-30% | 1-2% |
These numbers aren’t meant to scare you—they’re just facts that don’t always make it into the IVF brochure. If we’re weighing the morality, shouldn’t we ask: is it right to put moms and babies at risk for a chance at parenthood?
Interactive Quiz: What’s Your Take?
Let’s pause for a sec. How do you feel about these risks? Take this quick quiz:
- Does the higher chance of birth defects worry you?
- A) Yes, it’s a big deal.
- B) No, it’s worth the risk.
- Should women go through OHSS for a baby?
- A) No, it’s too much.
- B) Yes, if they choose to.
Jot down your answers and see where you land later. It’s a good way to check your gut on this stuff.
The Slippery Slope: Where Does IVF Lead?
Here’s something you won’t find in most articles: IVF opens the door to bigger ethical gray areas. Once you’re making embryos in a lab, what’s next? Preimplantation genetic testing (PGT) lets parents screen for diseases—or even pick traits like eye color. It’s already happening. A 2023 survey by the Pew Research Center found 15% of IVF users chose embryos based on non-medical traits. That’s designer babies territory.
Then there’s surrogacy, egg donation, and sperm banks. IVF makes it possible to have a baby with no biological tie to either parent—or with DNA from three people (yep, that’s a thing with mitochondrial donation). It’s not sci-fi; it’s today. The UK approved three-parent IVF in 2015, and it’s spreading.
This slippery slope worries people. If we’re cool with tweaking embryos now, what’s off-limits later? Cloning? Gene editing? A 2024 paper from the Hastings Center warned that unchecked IVF tech could lead to a “eugenics lite” future, where only the “best” embryos make the cut. That’s not a wild leap—it’s a pattern we’ve seen with other tech.
A Case Study: The Octomom Fallout
Remember Nadya Suleman, aka “Octomom”? In 2009, she had octuplets through IVF after a doctor implanted 12 embryos—way more than recommended. The kids survived, but the backlash was huge. Critics called it reckless, pointing to the health risks and the strain on her as a single mom. It’s an extreme example, but it shows how IVF can spiral when ethics take a backseat.
The Emotional Toll: Beyond the Lab
IVF isn’t just a physical or philosophical issue—it’s an emotional rollercoaster. Couples pour thousands of dollars (about $15,000 per cycle, says the American Pregnancy Association) and endless hope into it, only to face failure more often than success. The live birth rate for women under 35 is around 40%, dropping to 10% over 40. That’s a lot of heartbreak.
And what about the guilt? Parents who discard embryos sometimes wrestle with it for years. A 2023 study in Fertility and Sterility interviewed 50 IVF patients, and 30% said they felt conflicted about their unused embryos. One woman shared, “I couldn’t stop thinking they were my kids, even if they never grew.”
This emotional weight doesn’t get enough airtime. Clinics focus on success stories, but the failures—and the moral baggage—linger. Is it fair to put people through that?
Practical Tip: Coping with the Tough Stuff
If you or someone you know is considering IVF, here’s a game plan to handle the emotional side:
- Talk It Out: Find a counselor who gets infertility. It’s a safe space to vent.
- Set Limits: Decide upfront how many cycles you’ll try. It keeps hope from turning into obsession.
- Plan for Embryos: Think through what you’ll do with extras—freeze, donate, or let go—before you start.
These steps won’t erase the struggle, but they can make it less overwhelming.
The Social Divide: Who Gets IVF?
Here’s a point that’s flown under the radar: IVF isn’t equal opportunity. It’s expensive, and insurance rarely covers it fully. In the U.S., only 19 states mandate any coverage, per the National Conference of State Legislatures. That means it’s mostly for people who can pay out of pocket—often wealthier, white couples. A 2024 analysis by the CDC showed Black and Hispanic women use IVF at half the rate of white women, despite higher infertility rates.
This gap isn’t just unfair—it’s a moral issue. If IVF is a “right” to parenthood, why is it locked behind a paywall? And what does it say about us if only some get the chance? It’s a quiet inequity that deserves more noise.
Voting Time: Your Call
Should IVF be more accessible? Vote with your gut:
- ✔️ Yes, everyone deserves a shot at parenthood.
- ❌ No, it’s fine as a private choice.
No pressure—just a way to see where you stand.
A Fresh Angle: The Environmental Cost
Bet you haven’t thought about this: IVF has an environmental footprint. The labs, the shipping of frozen embryos, the disposable tools—it all adds up. A 2023 study from the University of California estimated that one IVF cycle produces about 50 pounds of medical waste and 500 pounds of CO2 emissions. Multiply that by the 300,000+ cycles in the U.S. each year, and it’s a climate concern nobody’s talking about.
In a world obsessed with going green, why does IVF get a pass? It’s not the main reason to question it, but it’s a layer that makes you think: how far are we willing to go for a baby?
Wrapping It Up: Where Do You Land?
IVF is a miracle for some and a moral mess for others. It’s a clash of science and soul—offering hope while raising questions about life, nature, and fairness. The embryo debate asks us to define humanity. The risks remind us nothing’s free. The slippery slope warns of a future we might not like. And the emotional and social costs hit closer to home than we admit.
So, where do you stand? Maybe you see IVF as a gift worth the trade-offs. Or maybe the ethical shadows give you pause. There’s no easy answer, but wrestling with it matters. Next time you hear about a “test-tube baby,” think beyond the headlines. What’s the real cost—and who’s paying it?
One Last Interactive Bit: Your Action Plan
Before you go, here’s a checklist to dig deeper:
- ✔️ Research local IVF stats—how many embryos are frozen near you?
- ✔️ Talk to someone who’s done it—what was their toughest call?
- ❌ Don’t just take my word—check out those studies yourself.
This isn’t about preaching; it’s about pondering. IVF’s here to stay, but the conversation’s just getting started. What’s your take?