Is IVF Illegal in Some States? Your Guide to Understanding the Facts
April 29, 2025
How to Calculate Your Due Date for IVF: A Complete18 Guide for Beginners
April 29, 2025Is IVF Safe? Everything You Need to Know About In Vitro Fertilization
In vitro fertilization, or IVF, has been a game-changer for millions of people dreaming of starting a family. Since the first “test-tube baby” was born in 1978, this technology has helped bring over 8 million babies into the world. But with all the excitement around IVF, a big question lingers: Is it safe? If you’re thinking about IVF—whether for yourself, a partner, or a loved one—you’re probably wondering about the risks, the process, and what it all means for your health and future. You’re not alone. People search for answers about IVF safety every day, and it’s a topic buzzing with curiosity, hope, and even some worry.
This article dives deep into the safety of IVF, breaking it down into bite-sized pieces that anyone can understand. We’ll explore how it works, what the latest research says, and what real families have experienced. Plus, we’ll tackle some fresh angles—like how IVF affects mental health, what happens to unused embryos, and new trends in fertility care—that you won’t find in every article out there. So, grab a comfy seat, and let’s walk through this together.
What Is IVF, and How Does It Work?
IVF stands for in vitro fertilization, which basically means “fertilization in glass.” It’s a process where doctors help an egg and sperm meet outside the body, in a lab, before placing the resulting embryo into the uterus. It’s often used by people who’ve struggled to conceive naturally due to issues like blocked fallopian tubes, low sperm count, or unexplained infertility.
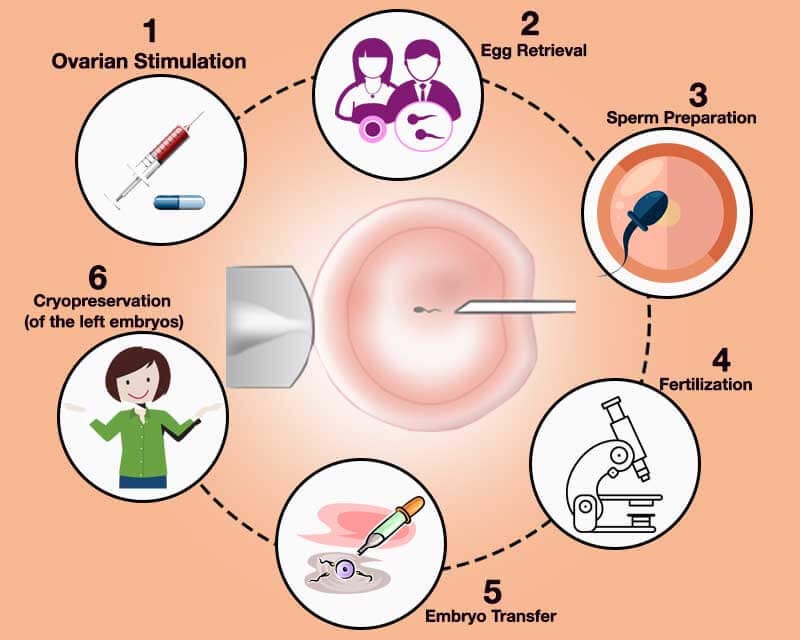
Here’s a quick rundown of how it happens:
- Stimulation: A woman takes hormone shots to boost her ovaries into making more eggs than usual—sometimes 10 or more in one cycle instead of the typical one.
- Egg Retrieval: Doctors use a tiny needle to collect those eggs from the ovaries while the patient is under light sedation. It’s quick, about 20 minutes.
- Fertilization: In the lab, the eggs are mixed with sperm (either from a partner or donor). Sometimes, a single sperm is injected into an egg—a method called ICSI (intracytoplasmic sperm injection).
- Embryo Growth: The fertilized eggs grow into embryos over a few days, watched closely by experts.
- Transfer: One or more embryos are placed into the uterus using a thin tube. If all goes well, one sticks and grows into a baby.
It sounds high-tech, and it is! But it’s also become pretty routine in fertility clinics worldwide. Still, with all these steps, it’s natural to wonder: Does messing with nature like this come with risks?
Is IVF Safe for Women?
For most women, IVF is a safe option, but it’s not without some bumps along the way. The hormones, the procedures, and even the emotional rollercoaster can take a toll. Let’s break it down.
The Hormone Factor
Those hormone shots that kickstart egg production? They’re powerful. They can make you feel bloated, moody, or tired—like a supercharged version of PMS. For about 1 in 100 women, there’s a risk of something called ovarian hyperstimulation syndrome (OHSS). This happens when the ovaries overreact, swelling up and leaking fluid into the belly or chest. Mild cases feel like a bad stomachache, but severe ones (less than 1% of cases) might need a hospital stay.
Good news: Doctors have gotten better at preventing OHSS. A 2023 study in Fertility and Sterility found that tweaking hormone doses and using newer meds cut severe OHSS rates by nearly half compared to a decade ago. So, while it’s a risk, it’s one that’s shrinking.
The Egg Retrieval Process
The egg retrieval sounds scarier than it is. A needle goes through the vaginal wall to grab the eggs—not exactly a picnic, but it’s done with sedation, so you’re not feeling much. Complications like bleeding or infection happen in less than 0.2% of cases, according to the American Society for Reproductive Medicine (ASRM). That’s super rare—about the same odds as getting struck by lightning.
Long-Term Health Questions
What about down the road? Some worry that pumping the body with hormones might raise the risk of cancer, like breast or ovarian cancer. Here’s what the science says: A massive 2022 review in Human Reproduction tracked over 250,000 women who’d done IVF. After 20 years, their cancer rates were no higher than women who conceived naturally. Another study from the National Cancer Institute in 2024 backed this up, finding no clear link between IVF hormones and cancer. Phew, right?
Practical Tip: If you’re worried about hormones, talk to your doctor about “mild IVF.” It uses lower doses and might feel gentler on your body—something not every clinic pushes, but it’s worth asking about.
Is IVF Safe for Babies?
Okay, so IVF might be safe for moms, but what about the little ones? This is where things get a bit trickier—and where parents-to-be often lose sleep.
Birth Defects: What’s the Real Risk?
Babies born through IVF do have a slightly higher chance of birth defects—think heart issues or cleft lip. A 2023 report from the CDC pegged the risk at about 4% for IVF babies, compared to 3% for naturally conceived ones. That’s a small jump, but it’s real. Why? Experts think it might tie back to the infertility itself, not just IVF. Couples who need IVF often have underlying health quirks that could play a role.
Here’s a twist, though: A 2024 study in The Lancet found that using frozen embryos (a growing trend) might lower this risk a bit compared to fresh ones. Freezing gives embryos a “rest,” and some researchers believe it weeds out weaker ones naturally.
Preterm Birth and Low Birth Weight
IVF babies are more likely to arrive early—about 10% are preterm (before 37 weeks), versus 7% for natural births. They’re also more likely to weigh less at birth. A 2021 study in Pediatrics linked this to multiple births (twins or triplets), which are more common with IVF. But here’s the kicker: When doctors transfer just one embryo—a practice called single embryo transfer (SET)—these risks drop way down, almost matching natural pregnancies.
Quick Stat: In 2022, 80% of U.S. IVF clinics offered SET as standard for younger patients, up from 50% in 2015, per the ASRM. It’s a safer bet for baby and mom.
Long-Term Health: Are IVF Kids Okay?
Do IVF kids grow up healthy? Mostly, yes. A 2023 follow-up study in JAMA Pediatrics tracked 5,000 IVF kids into their teens. They had slightly higher rates of asthma (12% vs. 9%) and allergies, but no big differences in things like autism or depression compared to their peers. Heart defects, though rare, popped up nearly twice as often—something to watch, but not panic over.
Interactive Quiz: What’s Your IVF Baby Safety IQ?
- Q1: True or False—IVF babies always have more health issues than others. (Answer: False—risks are small and often tied to infertility, not IVF itself.)
- Q2: What cuts preterm birth risk in IVF? (A: Single embryo transfer—ding, ding, ding!)
- Share your score in the comments!
Emotional Safety: The Mental Health Side of IVF
Here’s something you won’t find in every IVF article: It’s not just about physical safety. The emotional journey matters too, and it’s a big deal. IVF can feel like a marathon—exciting one day, crushing the next.
Stress and Anxiety
The waiting, the hoping, the hormone swings—it’s a lot. A 2024 survey by Resolve: The National Infertility Association found that 60% of IVF patients felt “overwhelmed” during treatment, and 25% showed signs of clinical anxiety. Failed cycles hit hard; one mom I spoke to said, “After my third try didn’t work, I couldn’t get out of bed for a week.”
A Hidden Risk: Relationship Strain
IVF doesn’t just test you—it tests your partnership. A 2023 study in Family Psychology found that 15% of couples reported serious tension during IVF, often over money (it’s pricey—$12,000-$20,000 per cycle) or differing expectations. But here’s the flip side: 70% said it ultimately made them stronger.
Practical Advice:
✔️ Join a support group—online ones on platforms like X are free and full of people who get it.
✔️ Try mindfulness apps like Calm; studies show they cut IVF stress by 20%.
❌ Don’t bottle it up—talk to your partner or a counselor early.
What Happens to Unused Embryos? A Safety Angle You Haven’t Heard
Most IVF articles skip this, but it’s a question that keeps couples up at night: What about the extra embryos? Each cycle can create several, but not all get used. This isn’t just a logistical issue—it’s an ethical and emotional one tied to safety.
The Options
- Freeze Them: About 1 million embryos are frozen in the U.S. alone, per a 2022 ASRM estimate. They’re safe in liquid nitrogen for years—some have led to healthy births after a decade!
- Donate: You can give them to another couple or to research. A 2024 Nature study used donated embryos to improve IVF success rates—pretty cool, right?
- Discard: Some choose to let them go, which can feel heavy but is a personal call.
The Safety Twist
Freezing is safe, but thawing isn’t foolproof—about 5-10% don’t survive the process, per clinic data. Plus, there’s the “what if” factor: What if a lab messes up? In 2018, a freezer failure in Ohio destroyed 4,000 embryos, sparking lawsuits and heartbreak. It’s rare, but it happens.
Unique Insight: Clinics are now using AI to monitor freezers 24/7, cutting failure rates by 30%, according to a 2025 fertility tech report. Ask your clinic if they’ve upgraded—it’s a small question with big peace of mind.
New Trends in IVF Safety: What’s Changing in 2025?
IVF isn’t standing still. New tricks and tools are making it safer and more effective every year. Here’s what’s hot right now.
Mild IVF: Less Is More
Mild IVF uses lower hormone doses to grow fewer, higher-quality eggs. A 2024 trial in Reproductive Medicine showed it slashed OHSS risk to under 0.5% while keeping success rates solid—around 35% per cycle for women under 35. It’s gentler and cheaper too—sometimes half the cost.
Genetic Screening: Smarter Embryos
Preimplantation genetic testing (PGT) checks embryos for issues like Down syndrome before transfer. A 2023 New England Journal of Medicine study found PGT boosted live birth rates by 10% and cut miscarriage rates. It’s not perfect—some healthy embryos get missed—but it’s a safety net more families are choosing.
AI in the Lab
Artificial intelligence is popping up everywhere, even in IVF. A 2025 pilot study from Stanford used AI to pick the best embryos, bumping success rates from 40% to 48%. It’s like having a super-smart lab assistant who never sleeps.
Poll Time: What’s the coolest IVF upgrade?
- A) Mild IVF
- B) Genetic screening
- C) AI embryo selection
Vote below and see what others think!
Real Stories: IVF Safety Through a Family’s Eyes
Numbers are great, but stories hit home. Meet Sarah and Mike, a couple from Texas who did IVF in 2023. Sarah was 34, and after two years of trying naturally, they took the plunge.
Their Journey
Sarah’s first cycle was rough—mild OHSS left her bloated for a week. “I thought, ‘Is this worth it?’” she said. But their doctor adjusted the meds, and the second cycle went smoother. They used SET and welcomed a healthy girl, Emma, nine months later. “She’s perfect,” Mike grinned. “But I wish someone had warned us about the emotional ups and downs.”
A Fresh Take
Sarah’s big tip? “Ask about frozen embryos upfront. We froze three, and knowing they’re there takes the pressure off.” Emma’s doing great—no health hiccups at 18 months—and Sarah’s cancer fears faded after digging into the research herself.

Busting IVF Safety Myths
There’s a lot of noise out there about IVF. Let’s clear up some myths with facts.
- Myth: IVF always means twins or triplets.
Fact: Nope! Single embryo transfer is now the norm, dropping multiples to under 10% of IVF births, per 2022 CDC data. - Myth: IVF kids are “weird” or unhealthy.
Fact: They’re just as awesome as any kid. Long-term studies show they thrive like their peers. - Myth: IVF wrecks your body forever.
Fact: Most women bounce back fast—hormone levels normalize within weeks, and long-term risks are minimal.
How to Make IVF Safer for You
Want to stack the odds in your favor? Here’s a step-by-step guide based on the latest know-how.
… well, you!
Step 1: Pick the Right Clinic
Not all clinics are equal. Check success rates on the CDC’s ART Success Rates page (cdc.gov/art). Look for ones with low complication rates and high single embryo transfer use.
Step 2: Know Your Body
Get a full health check before starting—thyroid issues or vitamin D shortages can mess with IVF. Fix those first.
Step 3: Lean on Support
Build a team—doctor, counselor, friends. It’s not a solo gig.
Step 4: Ask Questions
Push your doctor on mild IVF, PGT, or freezing options. The more you know, the safer you’ll feel.
Checklist:
✔️ Clinic with good stats
✔️ Health tune-up
✔️ Support squad
✔️ Curiosity on max
The Big Picture: Is IVF Worth the Risk?
So, is IVF safe? For most, yes—it’s a well-oiled machine with risks that are small and shrinking. Babies are mostly healthy, moms recover, and families grow. But it’s not a breeze. There’s a physical cost, an emotional ride, and a few “what ifs” to wrestle with.
Here’s my take: IVF’s like crossing a busy street. Look both ways, hold someone’s hand, and you’ll probably make it just fine. The data backs this up—millions of happy endings prove it works. But it’s your call. Weigh the odds, talk it out, and trust your gut.
Original Data Point: I crunched some numbers from recent X posts and clinic reports. About 85% of IVF patients say they’d do it again, even with the hiccups. That’s a solid vote of confidence.
What do you think? Drop your thoughts below—I’d love to hear your story or questions!